Back
Poster, Podium & Video Sessions
Moderated Poster
MP49: Urodynamics/Lower Urinary Tract Dysfunction/Female Pelvic Medicine: Basic Research & Pathophysiology
MP49-20: Urotypes in Young Women with Pelvic Pain: A Pilot Analysis of Clinical Urinary Microbiome Classification
Sunday, May 15, 2022
4:30 PM – 5:45 PM
Location: Room 228
James M. Weinberger*, L. Marcella Henao, Crystal Cisneros, James E. Ackerman, A. Lenore Ackerman, Los Angeles, CA

James M. Weinberger, MD, MBA
Fellow
UCLA
Poster Presenter(s)
Introduction: There are substantial differences in the urobiomes of women depending on age and menopausal status. Our previous work demonstrated that younger women (age <45) tended to have a more limited set of dominant microbes and could be classified by Next Generation Sequencing into one of 3 “urotypes” based on the composition of Lactobacilli and E. coli. We sought to determine if we could confirm that pattern in an unselected sampling of women seeking urogynecologic care and if these patterns correlated with presenting complaints.
Methods: Women (age 18-45) presenting with LUTS were prospectively enrolled if their clean-catch urine sample was deemed unnecessary for analysis by the provider. Samples were assessed via quantitative PCR (qPCR) for E. coli and Lactobacillus crispatus, gasseri, iners and jensenii and classified into urotypes using unsupervised clustering. The subset of women complaining of painful urogenital conditions were classified into the following categories using ICD-10 codes and primary provider-given diagnosis: bladder-specific pain syndrome (BPS), myofascial pelvic pain (MPP), and unspecified pelvic pain (PP). We performed correlations between bacterial types and pain diagnoses.
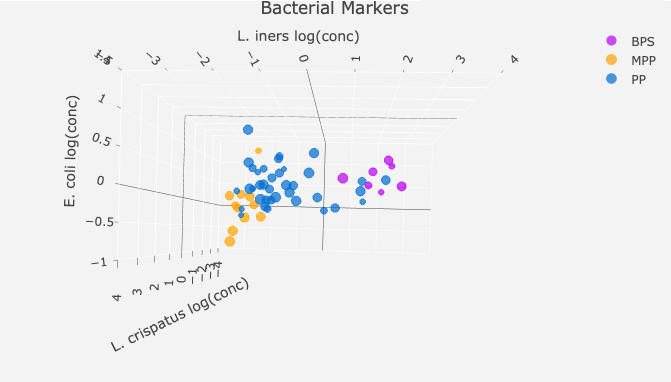
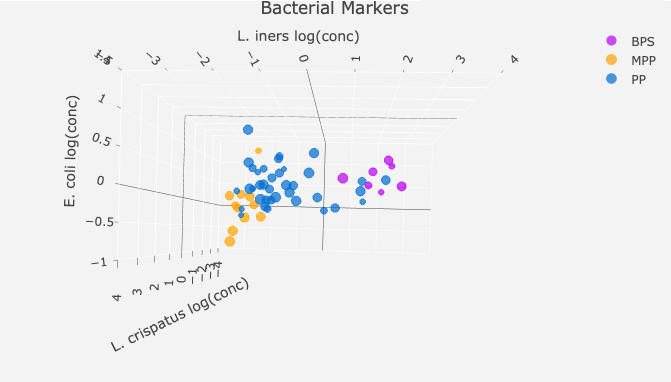
Results: Using Lactobacillus spp. and E. coli, premenopausal women could be classified into 3 dominant urotypes; the majority of asymptomatic subjects fell into Urotype 1(low Lactobacilli, low E. coli). Of the 186 premenopausal women enrolled, 56 were diagnosed with BPS, MPP, or PP. Examining across urotype, the MPP and BPS groups segregate; patients with MPP were Urotype 1, while BPS exhibited elevated L. iners (Urotype 2) (Figure 1). The majority of PP patients were Lactobacillus-poor, falling into the E.coli-positive urotype (Urotype 3).
Conclusions: Pelvic pain is a common complaint in this age group. While previous studies of pelvic pain have noted differences in diversity and Lactobacilli abundance between controls and pain groups, our qPCR-based urotyping was able to classify young women into three subgroups, demonstrating differential associations with asymptomatic controls and pelvic pain phenotypes. These data suggest that urotype data may be a meaningful mechanism to subclassify pelvic pain patients. Future studies are needed to determine if these groups correlate to treatment responses.
Source of Funding: N/a
Methods: Women (age 18-45) presenting with LUTS were prospectively enrolled if their clean-catch urine sample was deemed unnecessary for analysis by the provider. Samples were assessed via quantitative PCR (qPCR) for E. coli and Lactobacillus crispatus, gasseri, iners and jensenii and classified into urotypes using unsupervised clustering. The subset of women complaining of painful urogenital conditions were classified into the following categories using ICD-10 codes and primary provider-given diagnosis: bladder-specific pain syndrome (BPS), myofascial pelvic pain (MPP), and unspecified pelvic pain (PP). We performed correlations between bacterial types and pain diagnoses.
Results: Using Lactobacillus spp. and E. coli, premenopausal women could be classified into 3 dominant urotypes; the majority of asymptomatic subjects fell into Urotype 1(low Lactobacilli, low E. coli). Of the 186 premenopausal women enrolled, 56 were diagnosed with BPS, MPP, or PP. Examining across urotype, the MPP and BPS groups segregate; patients with MPP were Urotype 1, while BPS exhibited elevated L. iners (Urotype 2) (Figure 1). The majority of PP patients were Lactobacillus-poor, falling into the E.coli-positive urotype (Urotype 3).
Conclusions: Pelvic pain is a common complaint in this age group. While previous studies of pelvic pain have noted differences in diversity and Lactobacilli abundance between controls and pain groups, our qPCR-based urotyping was able to classify young women into three subgroups, demonstrating differential associations with asymptomatic controls and pelvic pain phenotypes. These data suggest that urotype data may be a meaningful mechanism to subclassify pelvic pain patients. Future studies are needed to determine if these groups correlate to treatment responses.
Source of Funding: N/a

.jpg)
.jpg)