Back
Poster, Podium & Video Sessions
Moderated Poster
MP50: Kidney Cancer: Localized: Surgical Therapy III
MP50-01: Prognostic impact of pathological renal parenchymal infiltration in non-metastatic clear cell renal cell carcinoma
Sunday, May 15, 2022
4:30 PM – 5:45 PM
Location: Room 225
Hajime Tanaka*, Yuki Fukawa, Kouhei Yamamoto, Shohei Fukuda, Sho Uehara, Soichiro Yoshida, Minato Yokoyama, Yoh Matsuoka, Tokyo, Japan, Steven C Campbell, Cleveland, OH, Yasuhisa Fujii, Tokyo, Japan
Hajime Tanaka, MD, PHD
Associate Professor
Tokyo Medical and Dental University
Poster Presenter(s)
Introduction: Previous studies highlighted the existence of heterogeneity in survival outcomes of patients with non-metastatic clear cell renal cell carcinoma (nmCCRCC), suggesting that further exploration is required to define high-risk patients. In this study, we investigated the prognostic impact of renal parenchymal infiltration (RPI) in nmCCRCC based on the pathological analysis with focus on the tumor interface with normal renal parenchyma.
Methods: We retrospectively analyzed 333 patients with nmCCRCC treated with radical nephrectomy. Two pathologists reviewed surgical specimens and determined the presence/absence of RPI, which was defined as tumor infiltration into the renal parenchyma by involving normal renal tissue and/or by forming small nests that were separate from the main lesion. Pathological TN stage (UICC version 8), microvascular invasion, and WHO/ISUP grade were also evaluated and the impacts of those parameters on recurrence-free survival (RFS) were analyzed.
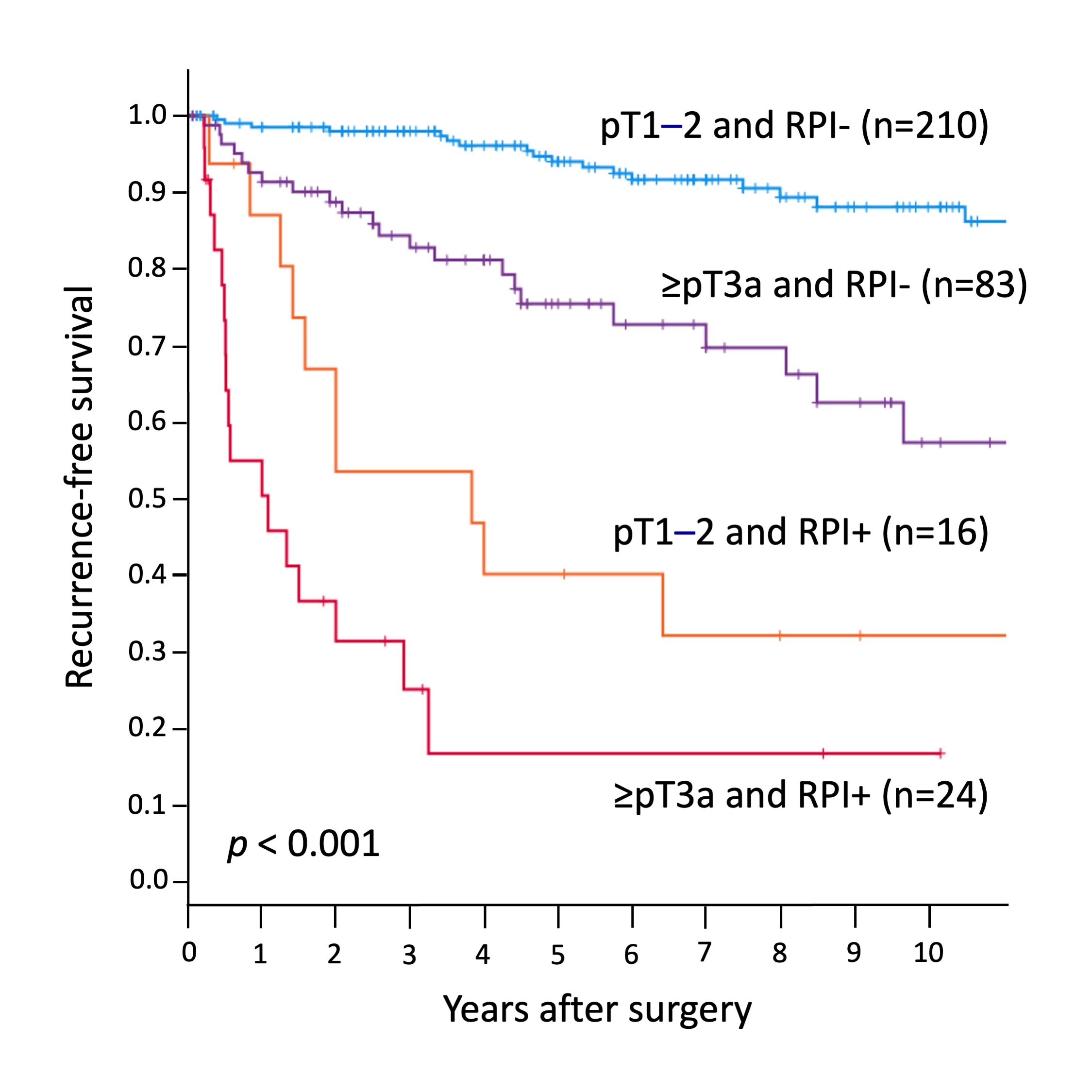
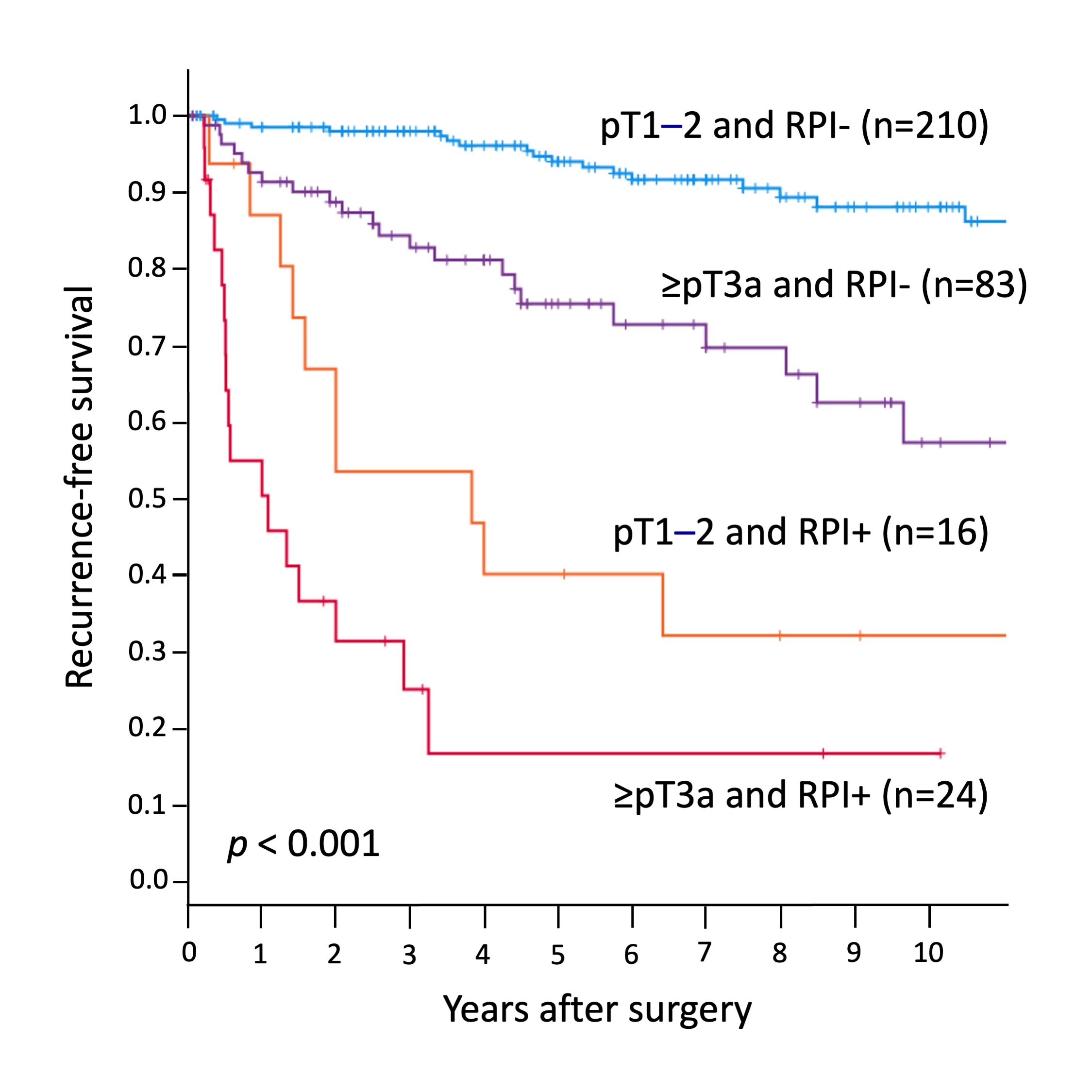
Results: The median age was 64 and 232 patients (70%) were male. The pathological analysis revealed invasions into perirenal fat, sinus fat, collecting system, and renal vein in 30 (9%), 33 (10%), 30 (9%), and 60 (18%) patients, respectively, resulting in 107 patients (32%) with =pT3a. Microvascular invasion was identified in 199 patients (60%) and 138 (41%) had WHO/ISUP grade 3-4. Overall 40 patients (12%), including 24 with =pT3a and 16 with pT1-2, were diagnosed with RPI.During the median follow-up of 6.0 years, 67 patients (20%) developed recurrence. In the multivariable analysis, =pT3a, microvascular invasion, WHO/ISUP grade 3-4, and RPI were independently associated with shorter RFS. The hazard ratio was highest for RPI (5.41 [95% CI: 3.10-9.44]) followed by microvascular invasion (3.04 [1.26-7.30]), WHO/ISUP grade (2.16 [1.20-3.87]), and =pT3a (2.13 [1.23-3.70]). According to pT stage and RPI, 5-year RFS was 17%, 40%, 76%, and 94% in the patients with =pT3a and RPI(+), pT1-2 and RPI(+), =pT3a and RPI(-), and pT1-2 and RPI(-), respectively (p < 0.001).
Conclusions: RPI is the primary determinant of poor prognosis in nmCCRCC among pathological parameters related to stage and grade. The presence of RPI predicts a high risk of recurrence early after surgery and adjuvant therapy may be considered for this population.
Source of Funding: None
Methods: We retrospectively analyzed 333 patients with nmCCRCC treated with radical nephrectomy. Two pathologists reviewed surgical specimens and determined the presence/absence of RPI, which was defined as tumor infiltration into the renal parenchyma by involving normal renal tissue and/or by forming small nests that were separate from the main lesion. Pathological TN stage (UICC version 8), microvascular invasion, and WHO/ISUP grade were also evaluated and the impacts of those parameters on recurrence-free survival (RFS) were analyzed.
Results: The median age was 64 and 232 patients (70%) were male. The pathological analysis revealed invasions into perirenal fat, sinus fat, collecting system, and renal vein in 30 (9%), 33 (10%), 30 (9%), and 60 (18%) patients, respectively, resulting in 107 patients (32%) with =pT3a. Microvascular invasion was identified in 199 patients (60%) and 138 (41%) had WHO/ISUP grade 3-4. Overall 40 patients (12%), including 24 with =pT3a and 16 with pT1-2, were diagnosed with RPI.During the median follow-up of 6.0 years, 67 patients (20%) developed recurrence. In the multivariable analysis, =pT3a, microvascular invasion, WHO/ISUP grade 3-4, and RPI were independently associated with shorter RFS. The hazard ratio was highest for RPI (5.41 [95% CI: 3.10-9.44]) followed by microvascular invasion (3.04 [1.26-7.30]), WHO/ISUP grade (2.16 [1.20-3.87]), and =pT3a (2.13 [1.23-3.70]). According to pT stage and RPI, 5-year RFS was 17%, 40%, 76%, and 94% in the patients with =pT3a and RPI(+), pT1-2 and RPI(+), =pT3a and RPI(-), and pT1-2 and RPI(-), respectively (p < 0.001).
Conclusions: RPI is the primary determinant of poor prognosis in nmCCRCC among pathological parameters related to stage and grade. The presence of RPI predicts a high risk of recurrence early after surgery and adjuvant therapy may be considered for this population.
Source of Funding: None

.jpg)
.jpg)