Back
Poster, Podium & Video Sessions
Moderated Poster
MP50: Kidney Cancer: Localized: Surgical Therapy III
MP50-02: How important are morphologic subtypes on the prognosis of surgically treated non-metastatic papillary renal cell carcinoma? An analysis from a contemporary multi-institutional database
Sunday, May 15, 2022
4:30 PM – 5:45 PM
Location: Room 225
Selcuk Erdem*, Istanbul, Turkey, Umberto Capitanio, Milan, Italy, Riccardo Campi, Florence, Italy, Daniele Amparore, Turin, Italy, Maria Carme Mir, Valencia, Spain, Eduard Roussel, Leuven, Belgium, Nicola Pavan, Trieste, Italy, Onder Kara, Kocaeli, Turkey, Tobias Klatte, Berlin, Germany, Enes Degirmenci, Resat Aydin, Istanbul, Turkey, Andrea Minervini, Sergio Serni, Alessandro Berni, Florence, Italy, Giacomo Rebez, Trieste, Italy, Faruk Ozcan, Istanbul, Turkey

Selcuk Erdem, MD
Urologic Oncology Division of Urology Department, Istanbul University Istanbul Faculty of Medicine
Poster Presenter(s)
Introduction: Papillary renal cell carcinoma (papRCC) is currently divided in 2 morphologic subtypes: type 1 and type 2. The aim of this contemporary multi-institutional study is to investigate the role of morphologic subtypes on the prognosis of surgically treated non-metastatic papRCC.
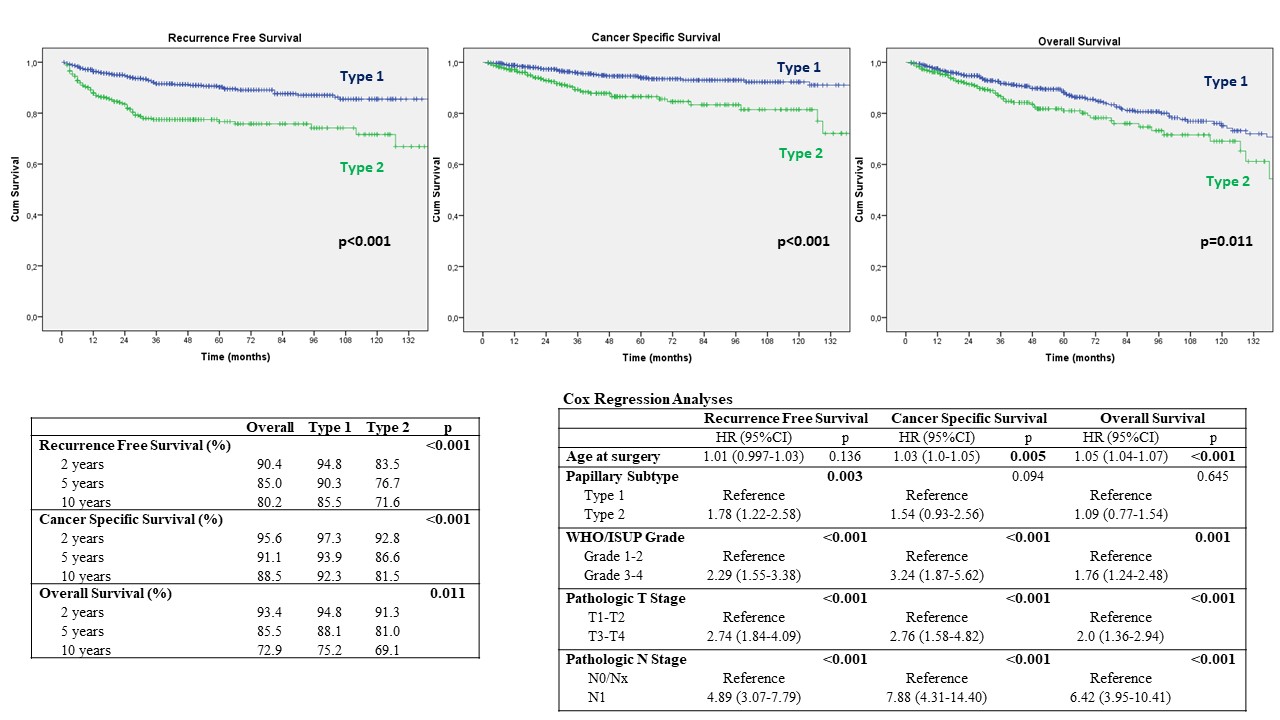
Methods: This study was conducted using a multi-institutional database consisting of 1219 patients with histopathologically confirmed non-metastatic papRCC after partial or radical nephrectomy collected from 8 tertiary European insitutions. The patients with accurate data for morphologic subtypes (type 1 and type 2) and follow-up records were included into this study. Clinical and histopathological parameters, recurrence free survival (RFS), cancer specific survival (CSS) and overall survival (OS) were compared between subtypes. Chi-square and Mann-Whitney U tests, and Kaplan-Meier survival analysis were used for the comparisons. Multivariable Cox Regression analysis was used to assess independent predictors on survival outcomes.
Results: A total of 879 patients were identified for this study. The patients in the type 2 group were older (64 vs. 66 years, p=0.006), had greater tumor size (3.8 vs. 4.3 cm, p=0.01) and more frequently underwent radical nephrectomy (25.7 vs. 35.2%, p=0.002). Nuclear grade (p < 0.001), pathologic T stage (p < 0.001) and N stage (p < 0.001) were significantly higher in the type 2 group. The median follow-up was 48 (IQR:24-88) months. Kaplan-Meier survival analyses showed that 5 year RFS (90.3% vs. 76.7%, p<0.001), CSS (93.9% vs. 86.6%, p<0.001) and OS (88.1% vs. 81.0%, p=0.011) were significantly lower in type 2 papRCC. Age, grade, pathologic T and N stage adjusted Cox-Regression analyses found that type 2 was independent predictor for RFS (HR:1.78 [95%CI:1.22-2.58], p=0.003), but not for CSS (HR:1.54 [95%CI:0.93-2.56], p=0.094) and OS (HR:1.09 [95%CI:0.77-1.54], p=0.645)
Conclusions: This contemporary multi-institutional study with a large dataset suggested that type 2 was associated with adverse histopathological outcomes, and was an independent predictor of RFS after surgical treatment of non-metastatic papRCC. These findings may guide decision making on follow-up schedule after surgery, and risk stratification for the adjuvant trials, in the individualized medicine era.
Source of Funding: None
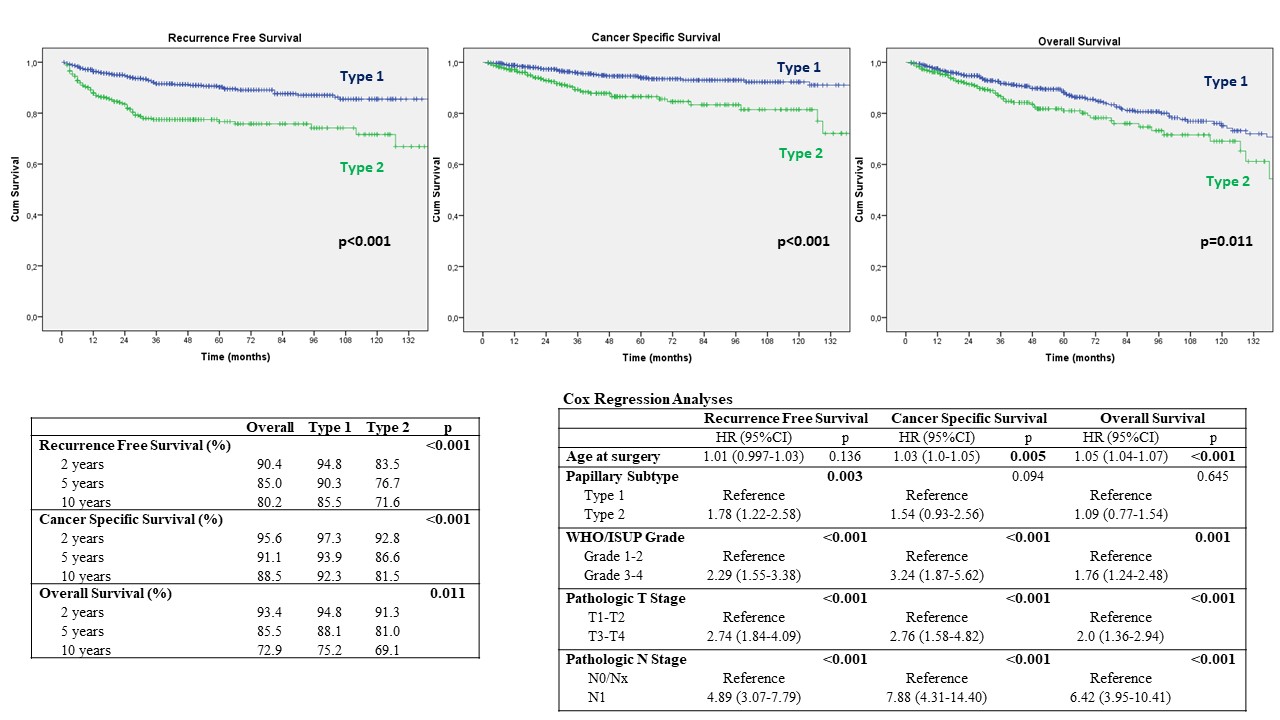
Methods: This study was conducted using a multi-institutional database consisting of 1219 patients with histopathologically confirmed non-metastatic papRCC after partial or radical nephrectomy collected from 8 tertiary European insitutions. The patients with accurate data for morphologic subtypes (type 1 and type 2) and follow-up records were included into this study. Clinical and histopathological parameters, recurrence free survival (RFS), cancer specific survival (CSS) and overall survival (OS) were compared between subtypes. Chi-square and Mann-Whitney U tests, and Kaplan-Meier survival analysis were used for the comparisons. Multivariable Cox Regression analysis was used to assess independent predictors on survival outcomes.
Results: A total of 879 patients were identified for this study. The patients in the type 2 group were older (64 vs. 66 years, p=0.006), had greater tumor size (3.8 vs. 4.3 cm, p=0.01) and more frequently underwent radical nephrectomy (25.7 vs. 35.2%, p=0.002). Nuclear grade (p < 0.001), pathologic T stage (p < 0.001) and N stage (p < 0.001) were significantly higher in the type 2 group. The median follow-up was 48 (IQR:24-88) months. Kaplan-Meier survival analyses showed that 5 year RFS (90.3% vs. 76.7%, p<0.001), CSS (93.9% vs. 86.6%, p<0.001) and OS (88.1% vs. 81.0%, p=0.011) were significantly lower in type 2 papRCC. Age, grade, pathologic T and N stage adjusted Cox-Regression analyses found that type 2 was independent predictor for RFS (HR:1.78 [95%CI:1.22-2.58], p=0.003), but not for CSS (HR:1.54 [95%CI:0.93-2.56], p=0.094) and OS (HR:1.09 [95%CI:0.77-1.54], p=0.645)
Conclusions: This contemporary multi-institutional study with a large dataset suggested that type 2 was associated with adverse histopathological outcomes, and was an independent predictor of RFS after surgical treatment of non-metastatic papRCC. These findings may guide decision making on follow-up schedule after surgery, and risk stratification for the adjuvant trials, in the individualized medicine era.
Source of Funding: None

.jpg)
.jpg)