Back
Poster, Podium & Video Sessions
Moderated Poster
MP50: Kidney Cancer: Localized: Surgical Therapy III
MP50-03: Systematic definition of treatment modality and clinical outcomes reporting system in case of surgical treatment for von hippel-lindau renal cell carcinoma
Sunday, May 15, 2022
4:30 PM – 5:45 PM
Location: Room 225
Alessandro Larcher, Federico Belladelli*, Andrea Ieva, Isaline Rowe, Giuseppe Fallara, Daniele Cignoli, Gianmarco Colandrea, Miriam Santangelo, Roberta Lucianò, Claudio Doglioni, Stefano Clerici, Laura Castellino, Anna Damascelli, Giorgia Guazzarotti, Francesco De Cobelli, Andrea Necchi, Daniele Raggi, Roberto Bertini, Francesco Montorsi, Umberto Capitanio, Andrea Salonia, Milan, Italy
- FB
Poster Presenter(s)
Introduction: Data on surgical treatment for Von Hippel-Lindau [VHL] renal cell carcinoma [RCC] is scarce because outcome reporting is extremely problematic: the same patient is diagnosed with multiple clear cell RCCs and receive multiple session of different treatment modalities over time. Since outcomes reporting system routinely applied to sporadic RCC is not applicable, the aim of the study is to propose a specific definition for treatment modality and clinical outcomes reporting system for VHL RCC
Methods: We propose to report baseline patient characteristic at the time of first surgery by defining each patient of the study population as a case, to report all the procedures performed on the study population during follow-up by defining each procedure as a case, to report cancer characteristics by defining each lesion as a case and finally to investigate time-dependent outcomes such as systemic progression or mortality starting from birth. We have applied such definition to the patients with a clinical or genetic VHL diagnosis enrolled in our prospective RCC database
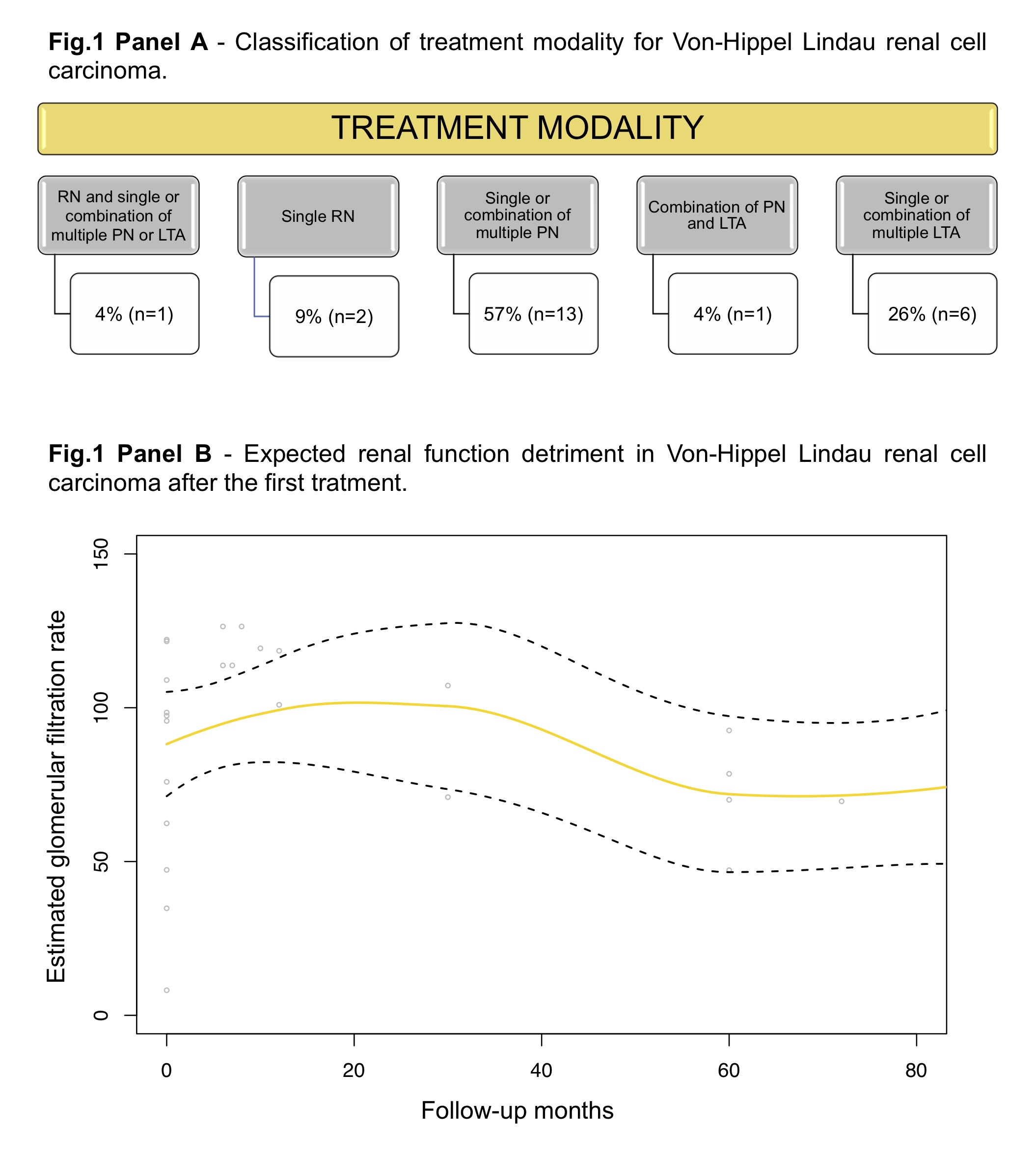
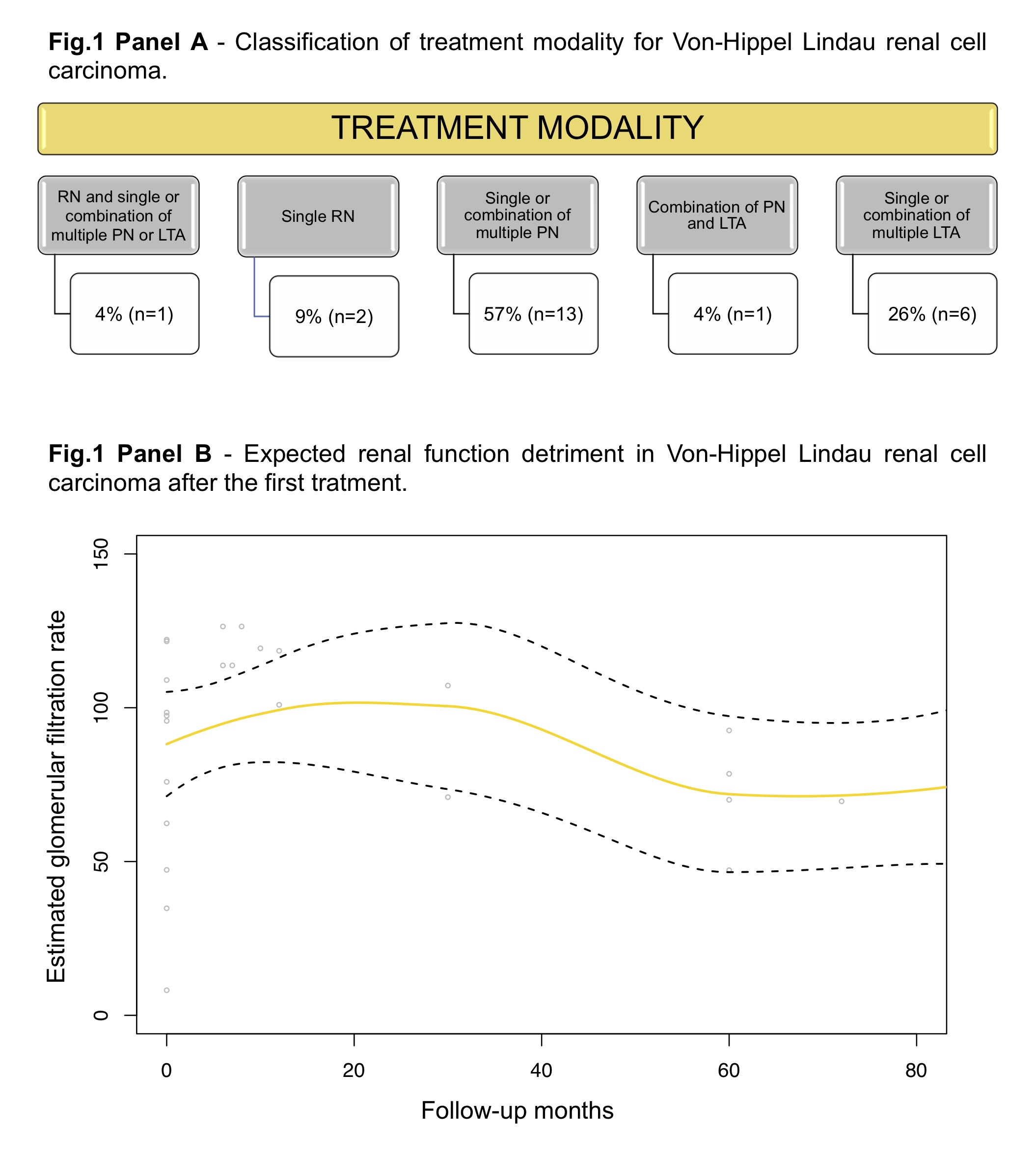
Results: Among 3,796 RCC patients elected for surgery, 0.3% had VHL. At first surgery, median age, preparative tumour size, and eGFR were 37 years, 3.0 cm and 100, respectively. During a median follow-up time of 72 months, the total number of procedures was 23 and the median number of procedures per patient was 2. Of those, 65% targeted only a lesion and 35% targeted multiple lesions. Treatment modalities are classified in Fig.1A. The median number of lesions per patient were 2 (2-3) and 39 lesions were treated in total. Of those, 100% resulted clear cell RCC and pathologic stage was pT1a, pT1b pT2 and pT3 in 64%, 28%, 5%, and 3% of cases, respectively. The overall and major complications rate per each surgical procedure were 22% and 9%. After a median follow-up of 81 months, median eGFR was 70 (Fig.1B). After 45 years from birth, 91% of the population was systemic progression free and 91% was alive
Conclusions: We have developed and applied for the first time a systematic definition of treatment modality and clinical outcomes reporting system in case of surgical treatment for VHL RCC. Such classification might improve the understanding of VHL RCC and the tracking of treatment outcomes
Source of Funding: no
Methods: We propose to report baseline patient characteristic at the time of first surgery by defining each patient of the study population as a case, to report all the procedures performed on the study population during follow-up by defining each procedure as a case, to report cancer characteristics by defining each lesion as a case and finally to investigate time-dependent outcomes such as systemic progression or mortality starting from birth. We have applied such definition to the patients with a clinical or genetic VHL diagnosis enrolled in our prospective RCC database
Results: Among 3,796 RCC patients elected for surgery, 0.3% had VHL. At first surgery, median age, preparative tumour size, and eGFR were 37 years, 3.0 cm and 100, respectively. During a median follow-up time of 72 months, the total number of procedures was 23 and the median number of procedures per patient was 2. Of those, 65% targeted only a lesion and 35% targeted multiple lesions. Treatment modalities are classified in Fig.1A. The median number of lesions per patient were 2 (2-3) and 39 lesions were treated in total. Of those, 100% resulted clear cell RCC and pathologic stage was pT1a, pT1b pT2 and pT3 in 64%, 28%, 5%, and 3% of cases, respectively. The overall and major complications rate per each surgical procedure were 22% and 9%. After a median follow-up of 81 months, median eGFR was 70 (Fig.1B). After 45 years from birth, 91% of the population was systemic progression free and 91% was alive
Conclusions: We have developed and applied for the first time a systematic definition of treatment modality and clinical outcomes reporting system in case of surgical treatment for VHL RCC. Such classification might improve the understanding of VHL RCC and the tracking of treatment outcomes
Source of Funding: no

.jpg)
.jpg)