Back
Poster, Podium & Video Sessions
Moderated Poster
MP50: Kidney Cancer: Localized: Surgical Therapy III
MP50-05: Order of thrombectomy for management of renal cell carcinoma with inferior vena cava thrombus
Sunday, May 15, 2022
4:30 PM – 5:45 PM
Location: Room 225
Yudai Ishiyama*, Tsunenori Kondo, Arakawa, Japan, Kazuhiko Yoshida, Junpei Iizuka, Kazunari Tanabe, Toshio Takagi, Tokyo, Japan

Yudai Ishiyama, MD
Tokyo Women's Medical University
Poster Presenter(s)
Introduction: Currently there is no consensus on whether to perform thrombectomy before kidney mobilization (“thrombus first”) or vice versa (“thrombus last”) for patients with renal cell carcinoma and inferior vena cava thrombus. The aim is to compare the perioperative outcomes between these two approaches.
Methods: We retrospectively evaluated 130 patients who underwent nephrectomy and thrombectomy at two institutions between 1992 and 2020. The cohort was classified into the thrombus-first and thrombus-last groups according to the order of the techniques used. Outcomes including the operative time, blood loss, and complications, especially the occurrence of intraoperative and postoperative pulmonary embolism, were compared.
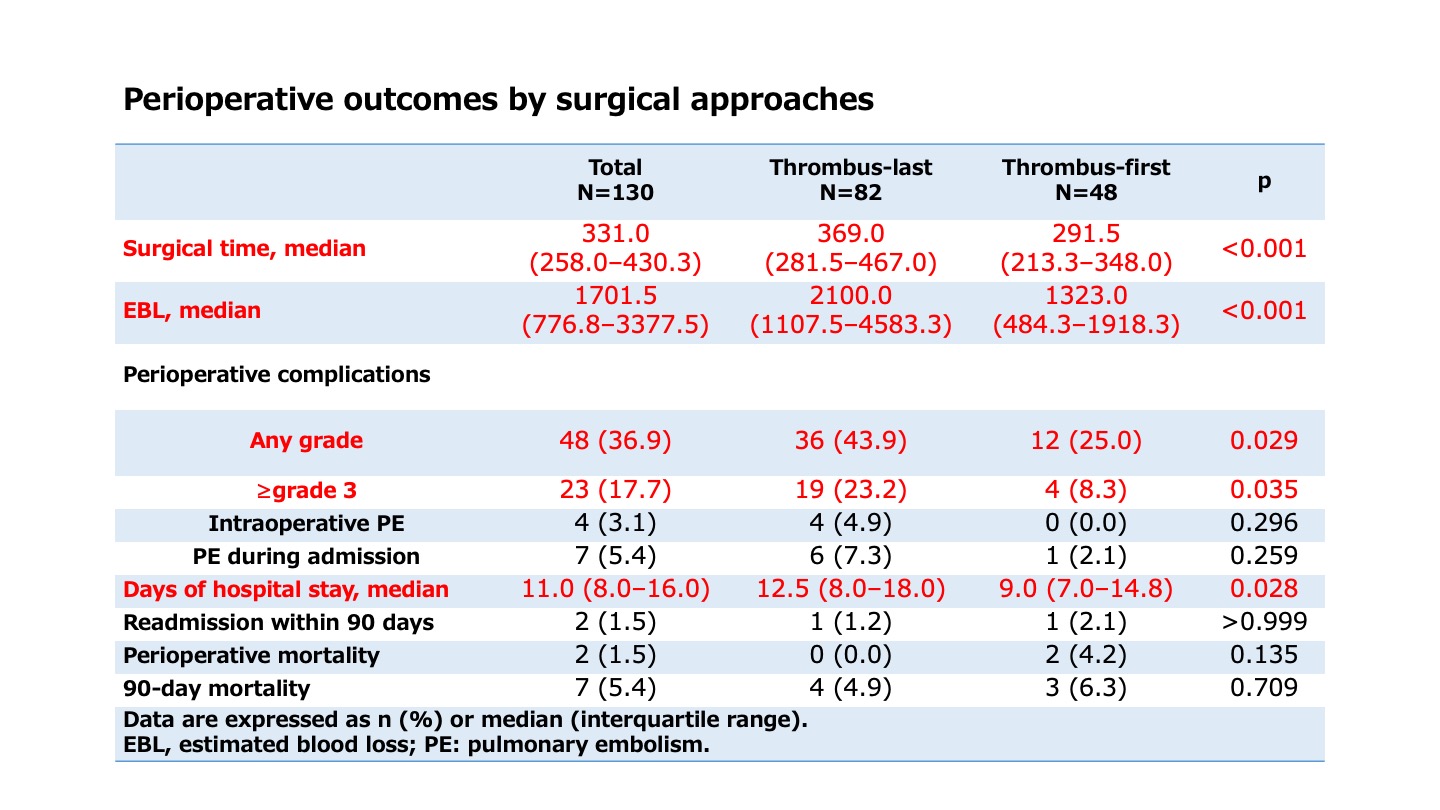
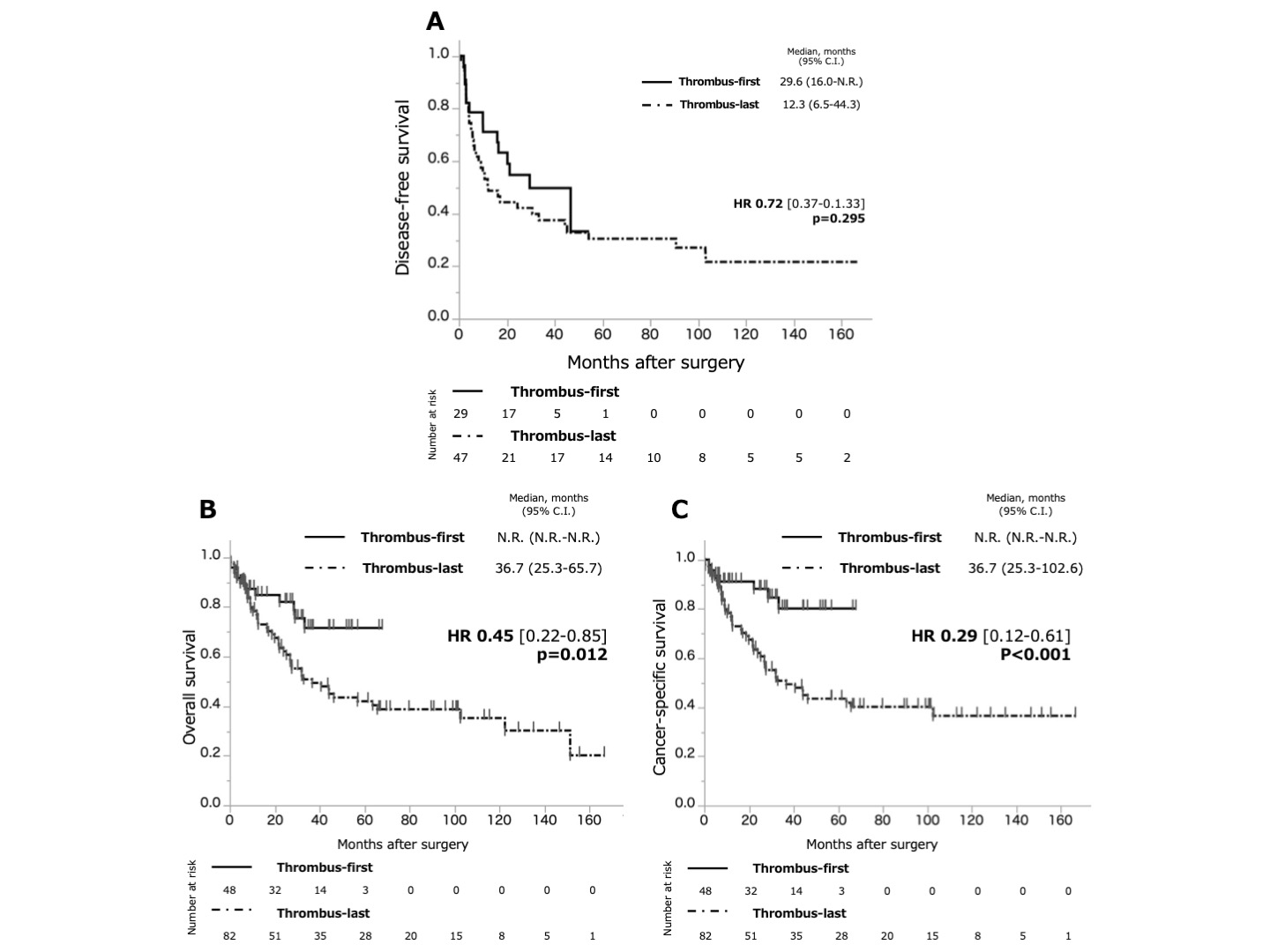
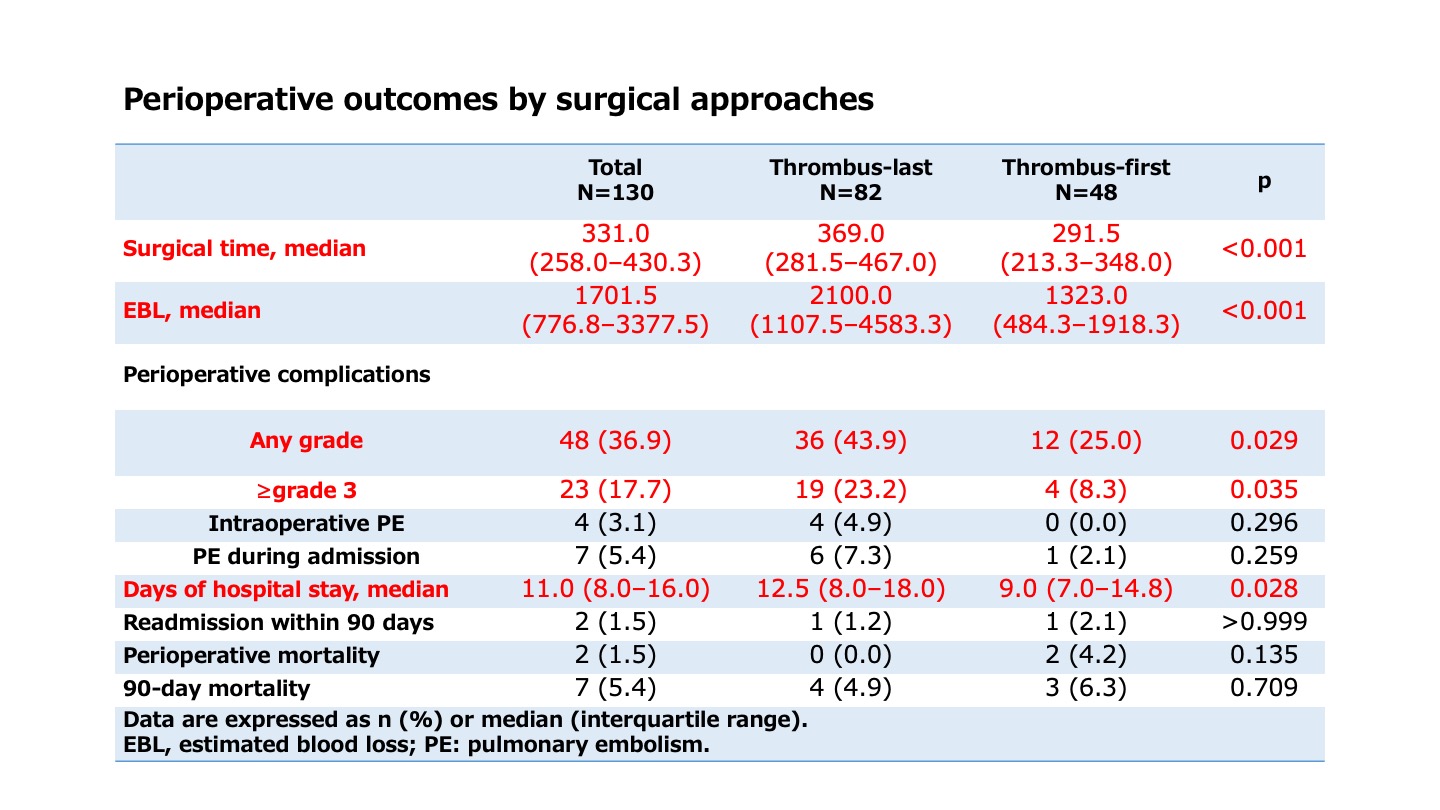
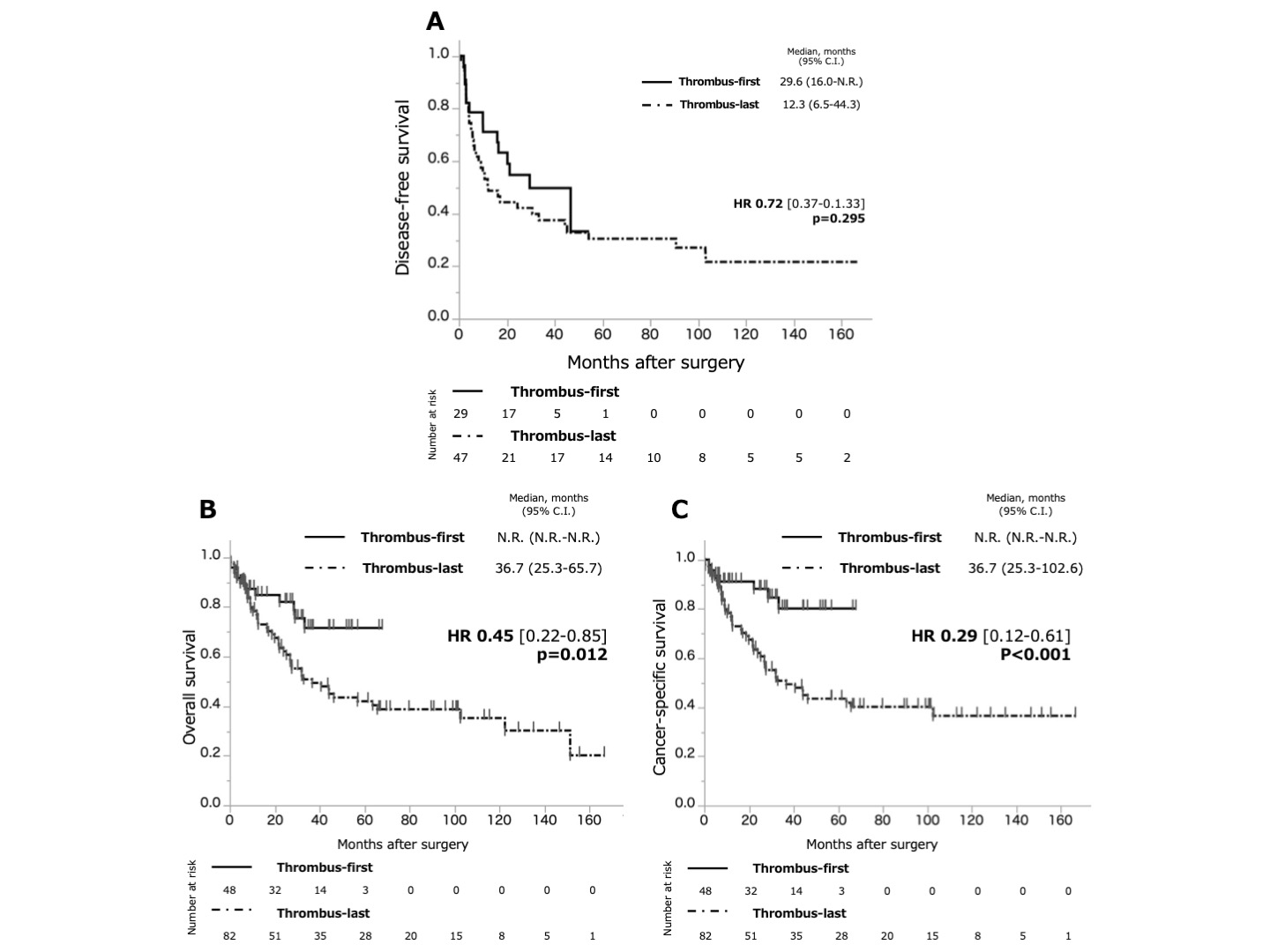
Results: The thrombus-first and thrombus-last groups comprised 48 and 82 patients, respectively. Characteristics such as age, performance status, Charlson Comorbidity Index, renal function, and level of tumour thrombus were comparable between the two groups. Approximately 41% of the patients had distant metastasis. There were four cases (3.1%) of intraoperative pulmonary embolism, all from the thrombus-last group. Seven patients overall (5.4%) experienced pulmonary embolism postoperatively with six in the thrombus-last group (7.3%) and one in the thrombus-first (2.1%) group (p=0.259). The surgical time (291.0 min vs. 369.0 min, p<0.001) and the blood loss (1323.0 mL vs. 2100.0 mL, p<0.001) were significantly smaller for the thrombus-first group than for the thrombus-last group. Occurrence of complications was 25.0% and 43.9% in thrombus-first and thrombus-last groups, respectively (p=0.029), and 8.3% and 23.2% for events graded =3 (p=0.035).
Conclusions: In surgery for renal cell carcinoma with inferior vena cava thrombus, performing thrombectomy before nephrectomy may serve to lessen complications, blood loss, and surgical time compared to nephrectomy before thrombectomy.
Source of Funding: None.
Methods: We retrospectively evaluated 130 patients who underwent nephrectomy and thrombectomy at two institutions between 1992 and 2020. The cohort was classified into the thrombus-first and thrombus-last groups according to the order of the techniques used. Outcomes including the operative time, blood loss, and complications, especially the occurrence of intraoperative and postoperative pulmonary embolism, were compared.
Results: The thrombus-first and thrombus-last groups comprised 48 and 82 patients, respectively. Characteristics such as age, performance status, Charlson Comorbidity Index, renal function, and level of tumour thrombus were comparable between the two groups. Approximately 41% of the patients had distant metastasis. There were four cases (3.1%) of intraoperative pulmonary embolism, all from the thrombus-last group. Seven patients overall (5.4%) experienced pulmonary embolism postoperatively with six in the thrombus-last group (7.3%) and one in the thrombus-first (2.1%) group (p=0.259). The surgical time (291.0 min vs. 369.0 min, p<0.001) and the blood loss (1323.0 mL vs. 2100.0 mL, p<0.001) were significantly smaller for the thrombus-first group than for the thrombus-last group. Occurrence of complications was 25.0% and 43.9% in thrombus-first and thrombus-last groups, respectively (p=0.029), and 8.3% and 23.2% for events graded =3 (p=0.035).
Conclusions: In surgery for renal cell carcinoma with inferior vena cava thrombus, performing thrombectomy before nephrectomy may serve to lessen complications, blood loss, and surgical time compared to nephrectomy before thrombectomy.
Source of Funding: None.

.jpg)
.jpg)