Back
Poster, Podium & Video Sessions
Moderated Poster
MP50: Kidney Cancer: Localized: Surgical Therapy III
MP50-07: Implications of Positive Surgical Margins following Robotic Partial Nephrectomy
Sunday, May 15, 2022
4:30 PM – 5:45 PM
Location: Room 225
Sij Hemal*, Mahmoud Abou Zeinab, Alp Tuna Beksac, Jayram Krishnan, cleveland, OH, Amr Fergany, Sebastian, FL, Robert Stein, Georges-Pascal Haber, Jihad Kaouk, cleveland, OH

Sij Hemal, MD
Cleveland Clinic Glickman Urological and Kidney Institute
Poster Presenter(s)
Introduction: Robotic Partial Nephrectomy (RPN) is a feasible approach for excising renal tumors of varying complexity while achieving good oncologic and functional outcomes. Expanding indications for RPN to complex renal masses raises concerns for compromising oncologic efficacy. Herein, we report the implications of positive surgical margins following RPN.
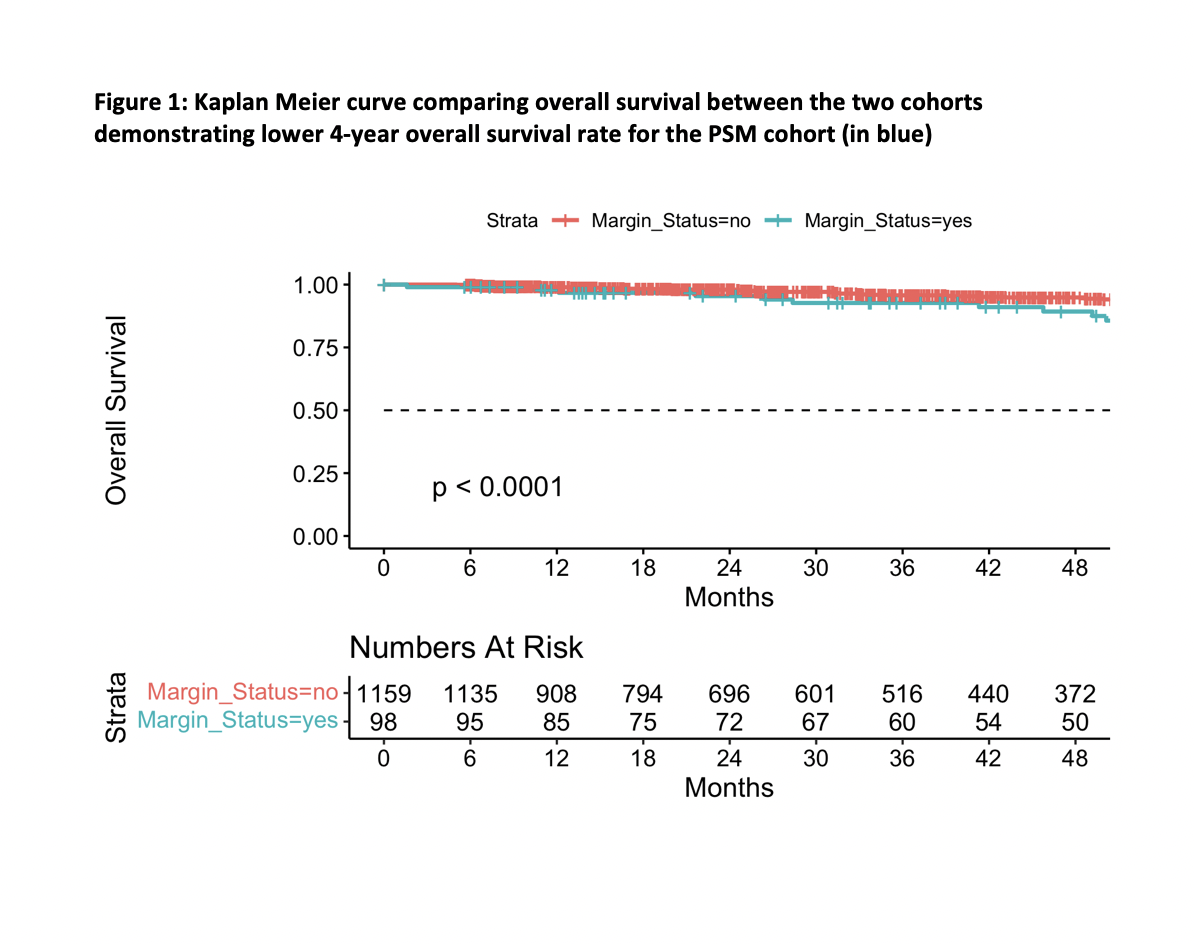
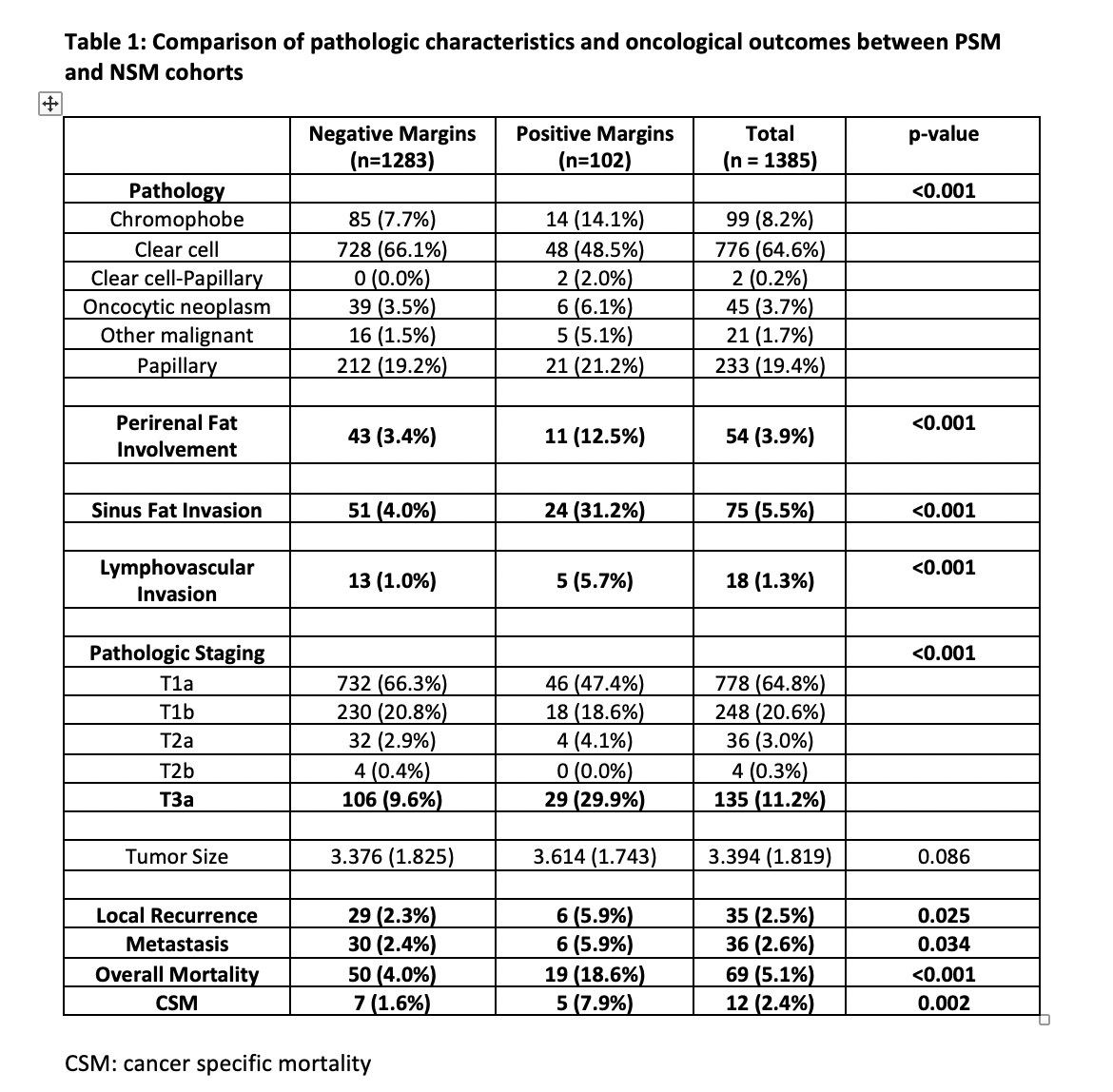
Methods: From a single center series, we retrospectively analyzed 1385 consecutive patients who underwent RPN from 2009-2020. Two cohorts were compared based on presence of positive surgical margin (PSM). All patients had at least 6 months follow-up. Groups were compared using chi-square for dichotomous variables and t-tests for continuous variables. A Kaplan-Meier method was performed to calculate the 4-year overall survival rate. Distant metastasis was defined as metastatic disease to brain, bone and lung. Associations between baseline characteristics and oncologic outcomes were assessed between the two groups.
Results: 1385 patients were included in our analysis (102 PSM and 1283 negative surgical margin (NSM)). The PSM group had a higher incidence of previous partial nephrectomy and a longer warm ischemia time (p-value < 0.05). From a pathologic standpoint, the PSM group had a greater incidence of pT3a pathology (30% vs 10%, p value < 0.001) as evidenced by higher rate of perirenal and sinus fat involvement (12.5% vs 3.4% and 31% vs 4% respectively, p value <0.001) and higher rate of lymphovascular invasion (5.7% vs 1 %, p value <0.001). From an oncological standpoint, PSM group had higher local recurrence rate (6% vs 2.3%, p value = 0.025) and greater distant metastasis rate (6% vs 2.4% p value = 0.034). Compared to the NSM cohort, at a mean follow up of 51 months, the PSM group had a greater overall mortality rate of 18.6% vs 4% (p-value <0.001) and cancer specific mortality of 7.9% vs 1.6% (p-value = 0.002).
Conclusions: PSM on final pathological evaluation is associated with an overall higher pathologic stage and confers a higher rate of local recurrence, distant metastasis and cancer specific mortality.
Source of Funding: None
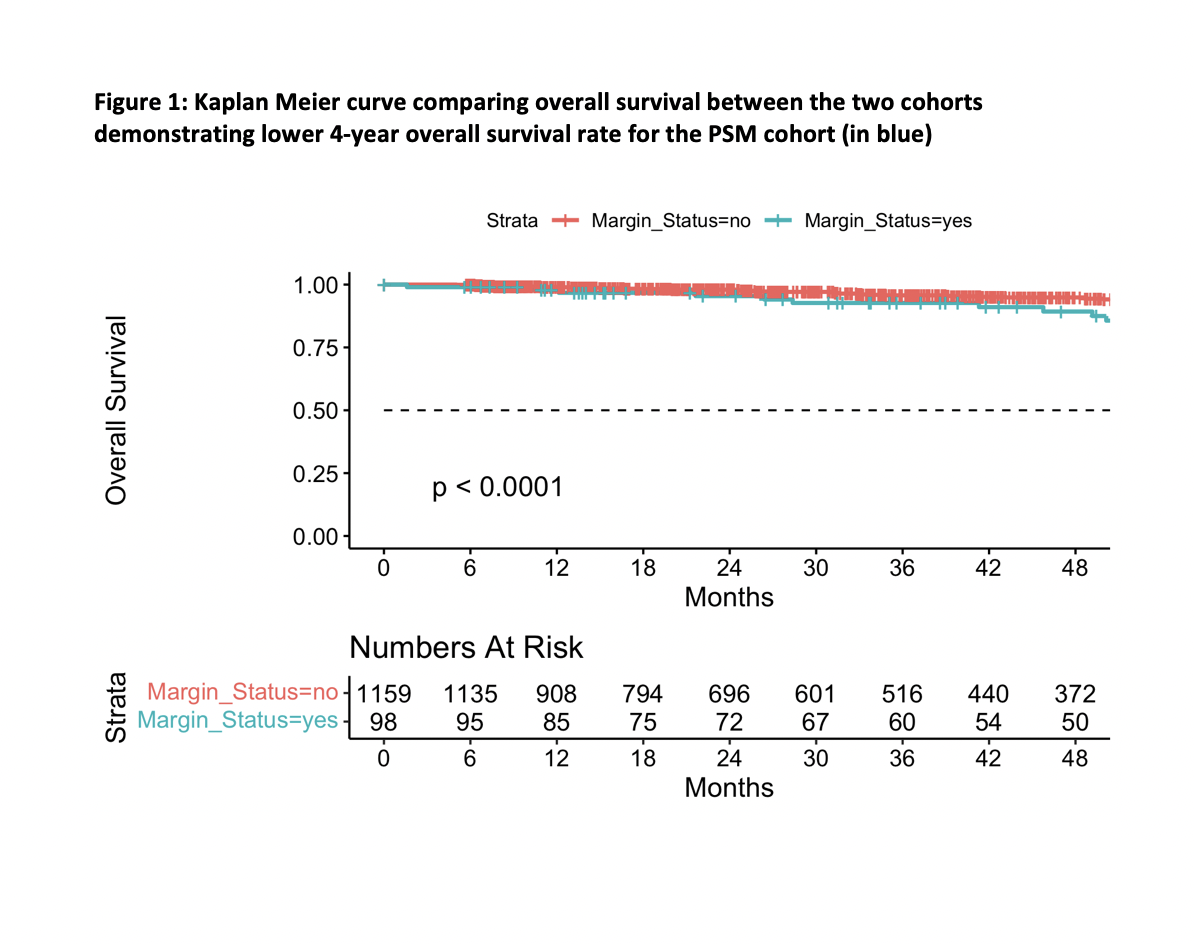
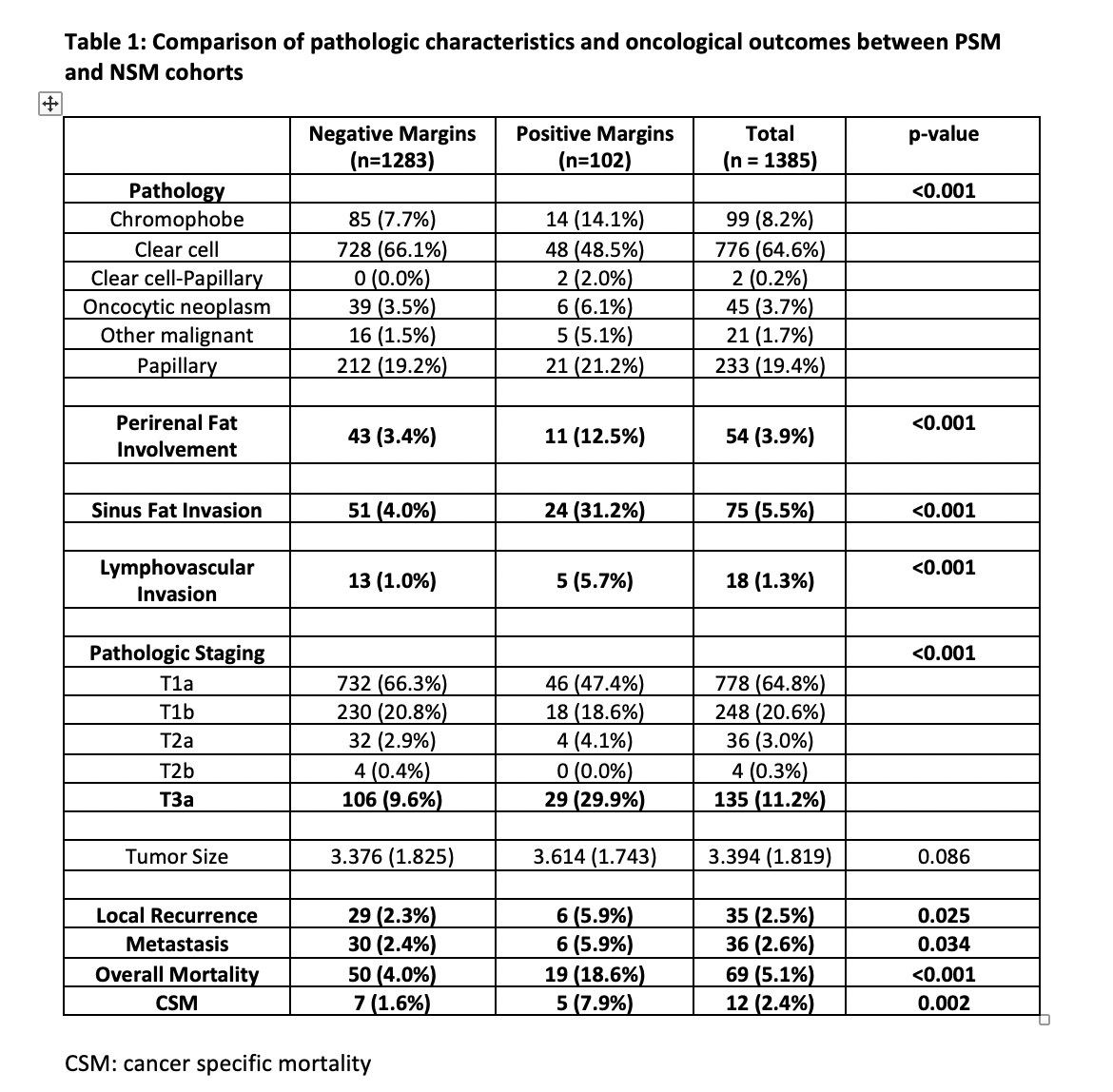
Methods: From a single center series, we retrospectively analyzed 1385 consecutive patients who underwent RPN from 2009-2020. Two cohorts were compared based on presence of positive surgical margin (PSM). All patients had at least 6 months follow-up. Groups were compared using chi-square for dichotomous variables and t-tests for continuous variables. A Kaplan-Meier method was performed to calculate the 4-year overall survival rate. Distant metastasis was defined as metastatic disease to brain, bone and lung. Associations between baseline characteristics and oncologic outcomes were assessed between the two groups.
Results: 1385 patients were included in our analysis (102 PSM and 1283 negative surgical margin (NSM)). The PSM group had a higher incidence of previous partial nephrectomy and a longer warm ischemia time (p-value < 0.05). From a pathologic standpoint, the PSM group had a greater incidence of pT3a pathology (30% vs 10%, p value < 0.001) as evidenced by higher rate of perirenal and sinus fat involvement (12.5% vs 3.4% and 31% vs 4% respectively, p value <0.001) and higher rate of lymphovascular invasion (5.7% vs 1 %, p value <0.001). From an oncological standpoint, PSM group had higher local recurrence rate (6% vs 2.3%, p value = 0.025) and greater distant metastasis rate (6% vs 2.4% p value = 0.034). Compared to the NSM cohort, at a mean follow up of 51 months, the PSM group had a greater overall mortality rate of 18.6% vs 4% (p-value <0.001) and cancer specific mortality of 7.9% vs 1.6% (p-value = 0.002).
Conclusions: PSM on final pathological evaluation is associated with an overall higher pathologic stage and confers a higher rate of local recurrence, distant metastasis and cancer specific mortality.
Source of Funding: None

.jpg)
.jpg)