Back
Poster, Podium & Video Sessions
Moderated Poster
MP50: Kidney Cancer: Localized: Surgical Therapy III
MP50-08: The prognostic significance of lymph node dissection in patients with non-metastatic renal cell carcinoma who underwent curative nephrectomy: A retrospective, long-term follow-up, multicenter study carcinoma (nmRCC) who underwent curative nephrectomy.
Sunday, May 15, 2022
4:30 PM – 5:45 PM
Location: Room 225
Sung Han Kim*, Jinsoo Chung, Hyung Ho Lee, Boram Park, Goyangsi, Korea, Republic of, Seok Soo Byun, Seongnamsi, Korea, Republic of, Chang Wook Chung, Sung Hoo Hong, Seoul, Korea, Republic of, Eu Chang Hwang, Hwasun, Korea, Republic of, Cheol Kwack, Seoul, Korea, Republic of
- SK
Poster Presenter(s)
Introduction: To evaluate the prognostic impact of lymph node dissection (LND) on recurrence-free survival (RFS), overall survival (OS), and cancer-specific survival (CSS) in patients with non-metastatic renal cell carcinoma (nmRCC) who underwent curative nephrectomy.
Methods: A retrospective, five-center study of 1328 nmRCC patients was performed between 2000 and 2012, and the patients were followed up until the end of 2018. Survival measures were compared according to the performance of the LND (LND vs. no LND groups) and the presence of node positivity (N+ and N- groups), while Kaplan-Meier analysis with the log-rank test and Cox regression analysis was used to determine the prognostic risk factors for each survival measure.
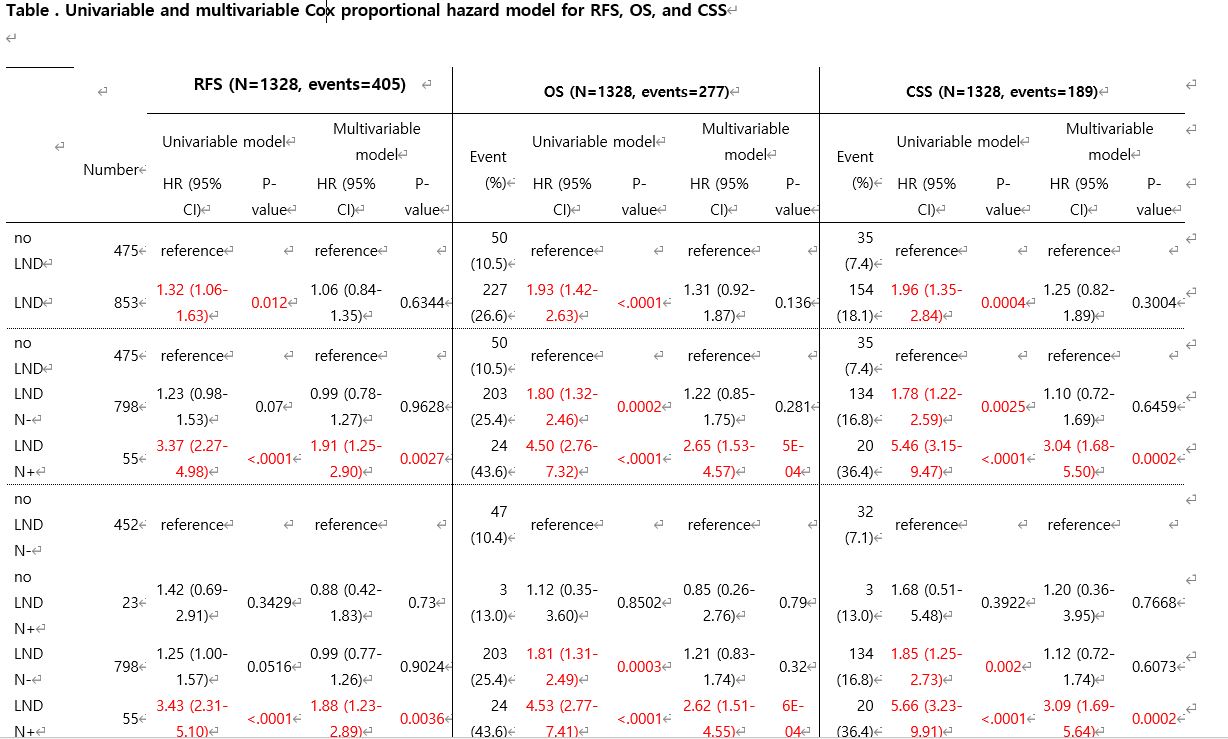
Results: During the median 55.8-month follow-up, 405 (30.5%) recurrences, 207 (15.6%) deaths, including 189 (14.0%) cancer-specific deaths, were recorded. The risk factor analyses showed that predictive factors for CSS and OS were similar, such as pathologic and clinical T stage, nuclear grade, European Cooperative Oncology Group Score, and albumin, neutrophil, and lymphocyte levels. Meanwhile, sarcomatoid differentiation was found as an additional predictive factor for CSS, while nephrectomy type and diabetes were found as additional predictive factors for OS (p < 0.05). For RFS, additional factors such as sarcomatoid differentiation, necrosis, and lymphovascular invasion were present and significant (p < 0.05). After adjusting for significant clinicopathological factors affecting survival outcomes considering the hazard ratios of each group in the multivariate analysis, the LND N+ group showed significantly worse prognoses for all survival types (p < 0.05). Meanwhile, in the no-LND and LND without positive nodal groups, there was no significant difference between any survival type. (p>0.05).
Conclusions: This study showed that nodal positivity significantly affected RFS, whereas LND significantly affected OS and CSS, in patients with nmRCC who underwent curative nephrectomy.
Source of Funding: None
Methods: A retrospective, five-center study of 1328 nmRCC patients was performed between 2000 and 2012, and the patients were followed up until the end of 2018. Survival measures were compared according to the performance of the LND (LND vs. no LND groups) and the presence of node positivity (N+ and N- groups), while Kaplan-Meier analysis with the log-rank test and Cox regression analysis was used to determine the prognostic risk factors for each survival measure.
Results: During the median 55.8-month follow-up, 405 (30.5%) recurrences, 207 (15.6%) deaths, including 189 (14.0%) cancer-specific deaths, were recorded. The risk factor analyses showed that predictive factors for CSS and OS were similar, such as pathologic and clinical T stage, nuclear grade, European Cooperative Oncology Group Score, and albumin, neutrophil, and lymphocyte levels. Meanwhile, sarcomatoid differentiation was found as an additional predictive factor for CSS, while nephrectomy type and diabetes were found as additional predictive factors for OS (p < 0.05). For RFS, additional factors such as sarcomatoid differentiation, necrosis, and lymphovascular invasion were present and significant (p < 0.05). After adjusting for significant clinicopathological factors affecting survival outcomes considering the hazard ratios of each group in the multivariate analysis, the LND N+ group showed significantly worse prognoses for all survival types (p < 0.05). Meanwhile, in the no-LND and LND without positive nodal groups, there was no significant difference between any survival type. (p>0.05).
Conclusions: This study showed that nodal positivity significantly affected RFS, whereas LND significantly affected OS and CSS, in patients with nmRCC who underwent curative nephrectomy.
Source of Funding: None

.jpg)
.jpg)