Back
Poster, Podium & Video Sessions
Moderated Poster
MP51: Prostate Cancer: Staging
MP51-12: The added value of microUS for the preoperative staging of prostate cancer: an update of a single-institutional prospective series
Sunday, May 15, 2022
4:30 PM – 5:45 PM
Location: Room 222
Vittorio Fasulo*, Edoardo Beatrici, Luca Disconzi, Pier Paolo Avolio, Nicola Frego, Pietro Diana, Marco Paciotti, Davide Maffei, Alessandro Uleri, Cesare Saitta, Paola Arena, Giuseppe Chiarelli, Andrea Gobbo, Milan, Italy, Alberto Saita, Rodolfo Hurle, Massimo Lazzeri, Milano, Italy, Giorgio Guazzoni, Milan, Italy, Paolo Casale, Milano, Italy, Nicolò Maria Buffi, Giovanni Lughezzani, Milan, Italy

Vittorio Fasulo, MD (he/him/his)
Humanitas University
Poster Presenter(s)
Introduction: A stratification of patients with prostate cancer (PCa) before robotic-assisted radical prostatectomy (RARP) allows performing a tailor-made surgery, providing a nerve-sparing procedure even in those patients with high-risk PCa. Since the accuracy of clinical parameters to determine extraprostatic extension (EPE) is moderate, there is urgent need for imaging tools capable of providing a more accurate assessment. Our goal is to evaluate the added value of microUS in the preoperative prediction of EPE.
Methods: This is a prospective single-institutional cohort study enrolling patients with biopsy-proven PCa scheduled for RARP. Patients with PSA>20ng/mL and prostate volume>100 mL were excluded. All patients underwent microUS prior to RARP.
MRI-derived features (curvilinear contact length (CCL), capsular bulging, visible extracapsular extension (ECE), as well as microUS features such as the presence of hypoechoic halo and obliteration of the vesicle-prostatic angle) were tested as predictors of EPE. Multivariable logistic regression models were fitted to test the accuracy of clinical parameters (total PSA, ISUP biopsy and digital rectal examination [DRE]) plus microUS parameters for the prediction of EPE.
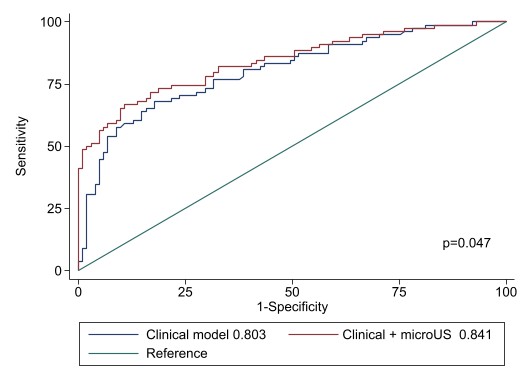
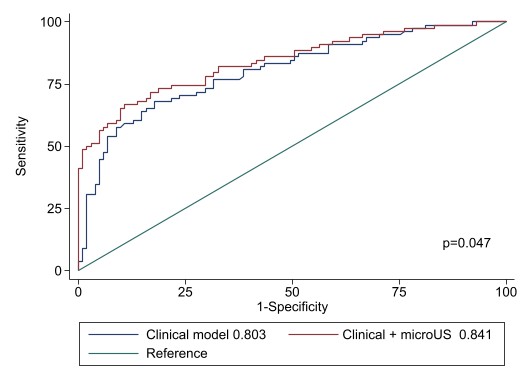
Results: Overall, 184 patients were prospectively recruited. Besides CCL, all predictors were associated with non-organ- confined disease (p < 0.001). Final pathology showed that 57.1% and 42.9% had respectively a pT2 and a pT3 or greater disease. The rate of non-organ-confined disease increased from 37.1%, in those individuals with only 1 predictor (OR 2.68), to 93.3% in those where 4 predictors were simultaneously observed (OR 63.5). At MLRM, the most significant risk factors for EPE were visible ECE (OR 5.21), positive DRE (OR 3.49), capsular bulge (OR 2.45), and PSA (OR 1.06). The clinical model alone showed an AUC of 0.804 as compared to 0.84 for the model including both clinical and microUS parameters (Figure1 ). The DeLong test for equality showed a difference between the two curves (p=0.0470).
Conclusions: Our findings suggest that microUS may represent an accurate tool for the evaluation of non-organ confined PCa. Future studies should externally validate our findings and determine the impact of this tool in the surgical and oncological outcomes of RARP.
Source of Funding: None
Methods: This is a prospective single-institutional cohort study enrolling patients with biopsy-proven PCa scheduled for RARP. Patients with PSA>20ng/mL and prostate volume>100 mL were excluded. All patients underwent microUS prior to RARP.
MRI-derived features (curvilinear contact length (CCL), capsular bulging, visible extracapsular extension (ECE), as well as microUS features such as the presence of hypoechoic halo and obliteration of the vesicle-prostatic angle) were tested as predictors of EPE. Multivariable logistic regression models were fitted to test the accuracy of clinical parameters (total PSA, ISUP biopsy and digital rectal examination [DRE]) plus microUS parameters for the prediction of EPE.
Results: Overall, 184 patients were prospectively recruited. Besides CCL, all predictors were associated with non-organ- confined disease (p < 0.001). Final pathology showed that 57.1% and 42.9% had respectively a pT2 and a pT3 or greater disease. The rate of non-organ-confined disease increased from 37.1%, in those individuals with only 1 predictor (OR 2.68), to 93.3% in those where 4 predictors were simultaneously observed (OR 63.5). At MLRM, the most significant risk factors for EPE were visible ECE (OR 5.21), positive DRE (OR 3.49), capsular bulge (OR 2.45), and PSA (OR 1.06). The clinical model alone showed an AUC of 0.804 as compared to 0.84 for the model including both clinical and microUS parameters (Figure1 ). The DeLong test for equality showed a difference between the two curves (p=0.0470).
Conclusions: Our findings suggest that microUS may represent an accurate tool for the evaluation of non-organ confined PCa. Future studies should externally validate our findings and determine the impact of this tool in the surgical and oncological outcomes of RARP.
Source of Funding: None

.jpg)
.jpg)