Back
Poster, Podium & Video Sessions
Moderated Poster
MP51: Prostate Cancer: Staging
MP51-13: Fluorine-18 (18F) prostate-specific membrane antigen (PSMA) positron emission tomography (PET) and the diagnosis and staging of primary prostate cancer (PCa)
Sunday, May 15, 2022
4:30 PM – 5:45 PM
Location: Room 222
Matthew Byrne*, Nithesh Ranasinha, Claudia Mercader, Mutie Raslan, Francesca Lewis, Stefanos Gorgoraptis, Ganesh Sathanapally, Ana Catarina Lopes Vieira, Golebka Jedrzej, Bryony Peiris, Mark Tuthill, Andrew Protheroe, Philip Camilleri, Phil Turner, Gerard Andrade, Saiful Miah, Tom Leslie, Richard Bryant, Freddie Hamdy, Ruth MacPherson, Fergus Gleeson, Alastair D. Lamb, Oxford, United Kingdom
- MB
Matthew Henry Vincent Byrne, MBBS MRes
University of Oxford
Poster Presenter(s)
Introduction: Recent studies have shown the superiority of PSMA-PET in staging of prostate cancer compared to conventional cross-sectional imaging. To date, most PSMA-PET scans have been performed for secondary prostate cancer and use a Gallium-68 ligand. Our objectives were to quantify local and distant staging by 18F PSMA PET in primary PCa.
Methods: We identified retrospectively a consecutive series of 18F PSMA-PET scans which we interrogated using a prospectively registered protocol (OSF registration ID: KTE3R). All PET scans were performed for staging of prostate cancer at a single UK tertiary referral centre, from the date of introduction of PSMA PET in September 2019 until August 2021. For primary staging, we compared PSMA PET to MRI and prostatectomy histology (for T and N staging), and MRI Marrow (for M staging).
Results: We identified 820 PSMA PET scans from 765 men, of which 354 were for primary staging. The mean age was 69.0 years (SD=7.4 years), and D’Amico risk classification was: 0.3% low risk; 72.0% intermediate risk; 27.7% high risk. We observed PSMA PET avidity in 96.9% of cases for local disease, 33.1% for nodal disease, and 32.5% for metastatic disease.
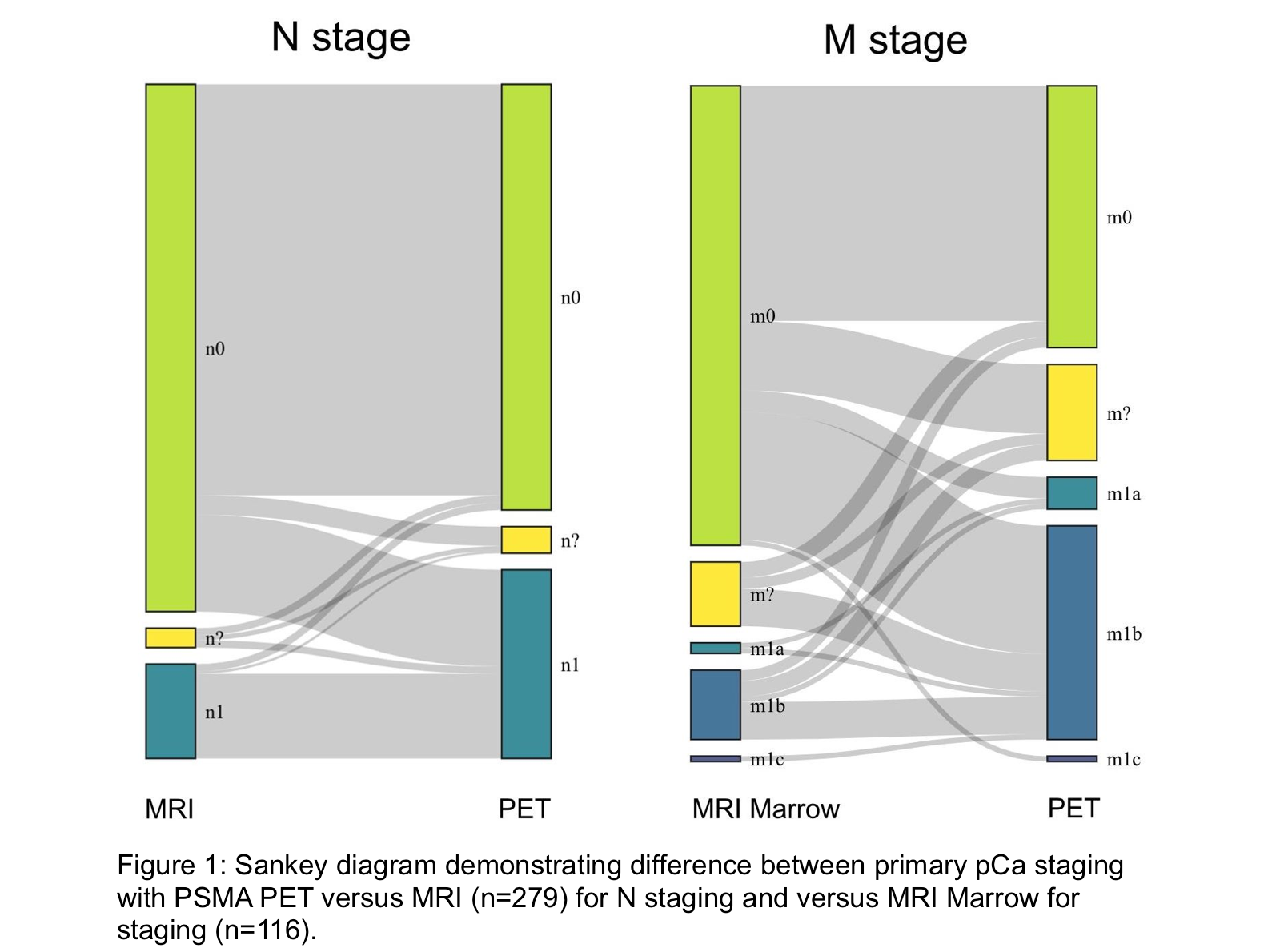
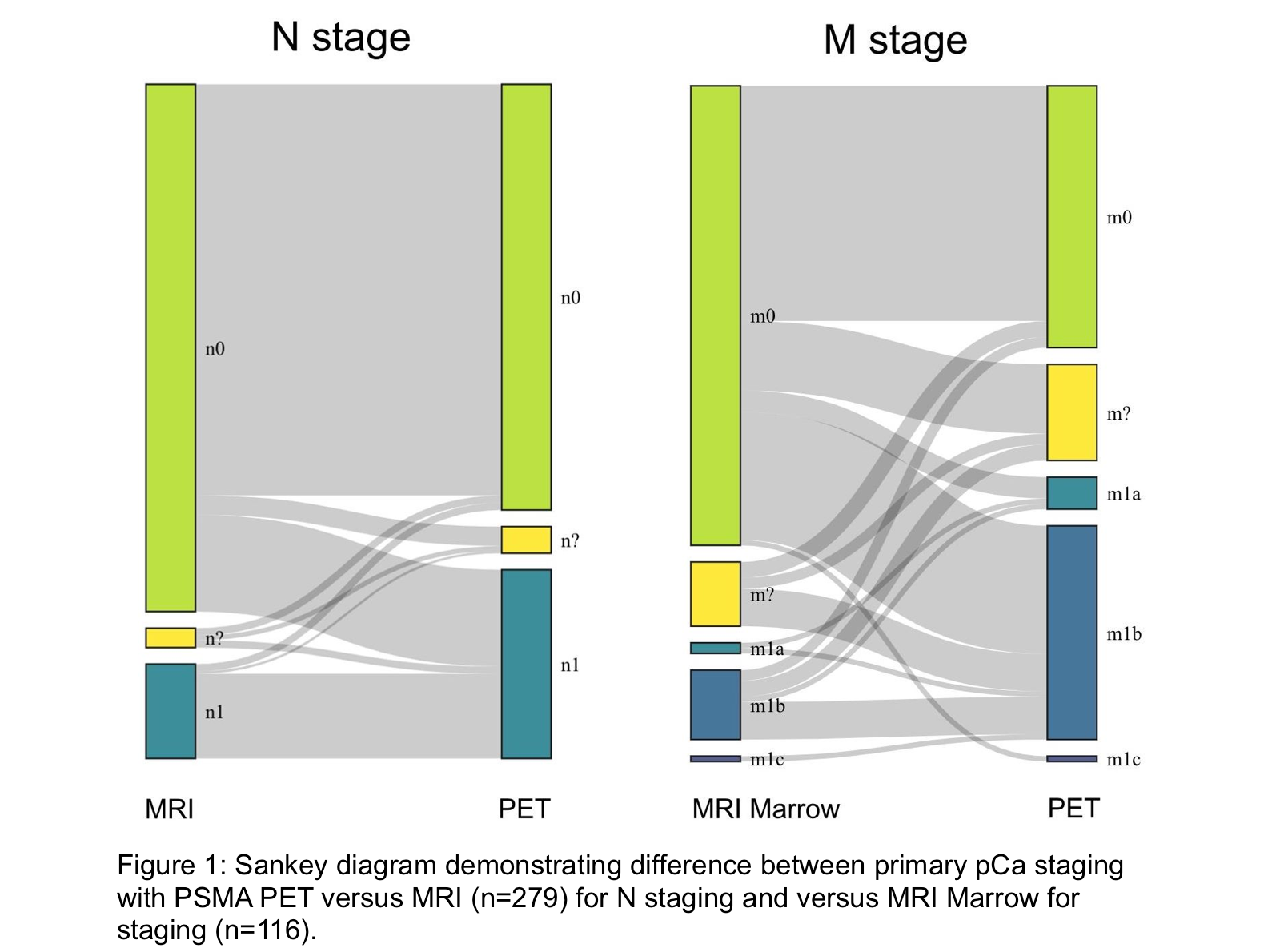
PSMA PET identified local disease similar to MRI (96.6% versus 96.9%, respectively), and identified 14.72% more nodal lesions than MRI, and 27.2% more metastatic lesions than MRI Marrow (Figure 1).
Some 47 men underwent radical prostatectomy after both PSMA-PET and MRI, of which all had positive histology. The sensitivity of PSMA-PET was 97.8% versus 93.6% with MRI for any primary lesion. A total of 21 of these patients had lymph node dissection, of which two had positive histology. The sensitivity of PSMA-PET for any nodal disease was 50% versus 0% with MRI.
Narrow slice MRI was used to corroborate skeletal lesions in 14 PSMA PET scans. None of the PSMA PET scans were positive on Narrow slice MRI, indicating an estimated false-positive rate for skeletal lesions of at least 6.7% (14 false positives versus 195 negative PSMA PET scans).
Conclusions: 18F PSMA-PET adds value over MRI in identification of local disease as well as nodal and distant metastatic spread. However, there is a notable estimated false-positive rate of at least 6.7%.
Source of Funding: None
Methods: We identified retrospectively a consecutive series of 18F PSMA-PET scans which we interrogated using a prospectively registered protocol (OSF registration ID: KTE3R). All PET scans were performed for staging of prostate cancer at a single UK tertiary referral centre, from the date of introduction of PSMA PET in September 2019 until August 2021. For primary staging, we compared PSMA PET to MRI and prostatectomy histology (for T and N staging), and MRI Marrow (for M staging).
Results: We identified 820 PSMA PET scans from 765 men, of which 354 were for primary staging. The mean age was 69.0 years (SD=7.4 years), and D’Amico risk classification was: 0.3% low risk; 72.0% intermediate risk; 27.7% high risk. We observed PSMA PET avidity in 96.9% of cases for local disease, 33.1% for nodal disease, and 32.5% for metastatic disease.
PSMA PET identified local disease similar to MRI (96.6% versus 96.9%, respectively), and identified 14.72% more nodal lesions than MRI, and 27.2% more metastatic lesions than MRI Marrow (Figure 1).
Some 47 men underwent radical prostatectomy after both PSMA-PET and MRI, of which all had positive histology. The sensitivity of PSMA-PET was 97.8% versus 93.6% with MRI for any primary lesion. A total of 21 of these patients had lymph node dissection, of which two had positive histology. The sensitivity of PSMA-PET for any nodal disease was 50% versus 0% with MRI.
Narrow slice MRI was used to corroborate skeletal lesions in 14 PSMA PET scans. None of the PSMA PET scans were positive on Narrow slice MRI, indicating an estimated false-positive rate for skeletal lesions of at least 6.7% (14 false positives versus 195 negative PSMA PET scans).
Conclusions: 18F PSMA-PET adds value over MRI in identification of local disease as well as nodal and distant metastatic spread. However, there is a notable estimated false-positive rate of at least 6.7%.
Source of Funding: None

.jpg)
.jpg)