Back
Poster, Podium & Video Sessions
Moderated Poster
MP51: Prostate Cancer: Staging
MP51-15: The role of 68Ga-PSMA- and 68Ga-DOTA-RM2 PET/MRI in the primary staging of high-risk Prostate Cancer patients undergoing radical prostatectomy. Preliminary results of a prospective, single center study.
Sunday, May 15, 2022
4:30 PM – 5:45 PM
Location: Room 222
Vito Cucchiara, Paola Mapelli*, Samuele Ghezzo, Ana Maria Samanes Gajate, Enrico Camisassa, Sabrina Comana, Erik Preza, Giorgio Brembilla, Naghia Ahmed, Carolina Bezzi, Luca Presotto, Valentino Bettinardi, Annarita Savi, Patrizia Magnani, Raffaele Menichini, Angela Coliva, Ilaria Neri, Ettore Di Gaeta, Luigi Gianolli, Giorgio Gandaglia, Francesco Montorsi, Alberto Briganti, Francesco De Cobelli, Paola Scifo, Maria Picchio, Milan, Italy
- PM
Poster Presenter(s)
Introduction: PSMA PET/MRI is an option for staging of newly diagnosed high-risk prostate cancer (PCa) patients. However, PSMA might still miss micro-metastatic disease. 68Ga-DOTA-RM2 (bombesin) is a promising tracer for PET imaging of PCa, but limited data are currently available. We hypothesized that the combined use of PET and MRI with these tracers could improve staging. We aimed at investigating the synergic role of 68Ga-PSMA PET/MRI and 68Ga-DOTA-RM2 PET/MRI in the primary staging of high-risk PCa.
Methods: 22 patients with biopsy proven PCa were enrolled in this prospective trial (EudraCT: 2018-001034-18). All men had high-risk PCa. Prior to RP, all patients underwent 68Ga-PSMA PET/MRI and 19/22 underwent 68Ga-DOTA-RM2 PET/MRI within 16 days. TNM classification based on imaging findings was performed. Semi-quantitative PET and quantitative MRI parameters were collected. DICE score between regions of interest manually segmented on the primary tumor on 68Ga-DOTA-RM2 PET, 68Ga-DOTA-RM2 PET and on T2 MRI was computed. Pathological specimens of 14/22 patients were collected and used as gold standard to validate intra-prostatic findings. Fisher’s exact test and Mann-Whitney U test were used to compare groups.
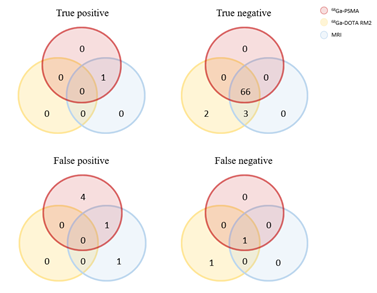
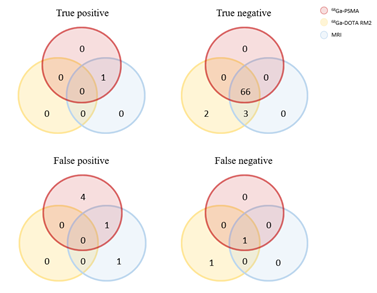
Results: All imaging modalities detected the primary PCa in 18/19 patients. In 16/19 patients the site of the primary prostatic lesion was concordant among the three imaging modalities. SVI was detected by MRI in 7 patients, by 68Ga-PSMA in 2 patients while no case of SVI was detected by 68Ga-DOTA-RM2. 68Ga-PSMA images revealed cN1 disease in 7/22 patients and bone metastases in 3/22. At 68Ga-DOTA-RM2 PET a pathological focal uptake was detected at nodal and skeletal level in 4/19 and no patients. Figure 1 reports the Venn diagram for lymph node involvement for all imaging modalities using histopathological specimens at per-node analysis.
Conclusions: 68Ga-PSMA and 68Ga-DOTA- RM2 PET/MRI might be useful in PCa staging. Based on preliminary data, a synergic role of 68Ga-PSMA PET and mpMRI for primary PCa characterization might be hypothesized. 68Ga-DOTA-RM2 PET/MRI was inferior to 68Ga-PSMA PET/MRI in terms of local and distant staging.
Source of Funding: None.
Methods: 22 patients with biopsy proven PCa were enrolled in this prospective trial (EudraCT: 2018-001034-18). All men had high-risk PCa. Prior to RP, all patients underwent 68Ga-PSMA PET/MRI and 19/22 underwent 68Ga-DOTA-RM2 PET/MRI within 16 days. TNM classification based on imaging findings was performed. Semi-quantitative PET and quantitative MRI parameters were collected. DICE score between regions of interest manually segmented on the primary tumor on 68Ga-DOTA-RM2 PET, 68Ga-DOTA-RM2 PET and on T2 MRI was computed. Pathological specimens of 14/22 patients were collected and used as gold standard to validate intra-prostatic findings. Fisher’s exact test and Mann-Whitney U test were used to compare groups.
Results: All imaging modalities detected the primary PCa in 18/19 patients. In 16/19 patients the site of the primary prostatic lesion was concordant among the three imaging modalities. SVI was detected by MRI in 7 patients, by 68Ga-PSMA in 2 patients while no case of SVI was detected by 68Ga-DOTA-RM2. 68Ga-PSMA images revealed cN1 disease in 7/22 patients and bone metastases in 3/22. At 68Ga-DOTA-RM2 PET a pathological focal uptake was detected at nodal and skeletal level in 4/19 and no patients. Figure 1 reports the Venn diagram for lymph node involvement for all imaging modalities using histopathological specimens at per-node analysis.
Conclusions: 68Ga-PSMA and 68Ga-DOTA- RM2 PET/MRI might be useful in PCa staging. Based on preliminary data, a synergic role of 68Ga-PSMA PET and mpMRI for primary PCa characterization might be hypothesized. 68Ga-DOTA-RM2 PET/MRI was inferior to 68Ga-PSMA PET/MRI in terms of local and distant staging.
Source of Funding: None.

.jpg)
.jpg)