Back
Poster, Podium & Video Sessions
Moderated Poster
MP51: Prostate Cancer: Staging
MP51-16: The Risk of Recurrence in cN1 Prostate Cancer Patients treated with radical prostatectomy Varies According to the type Preoperative Staging. A comparison between 68Ga-PSMA-PET versus Conventional Imaging in a large, Multi-institutional Study
Sunday, May 15, 2022
4:30 PM – 5:45 PM
Location: Room 222
Gabriele Sorce*, Milan, Italy, Giuseppe Rosiello, Milano, Italy, Giorgio Gandaglia, Milan, Italy, Simone Scuderi, Milano, Italy, Lorenzo Bianchi, Riccardo Schiavina, Bologna, Italy, Bram Vansevenant, Gaëtan Devos, Leuven, Belgium, Armando Stabile, Riccardo Leni, Daniele Robesti, Elio Mazzone, Antony Pellegrino, Milano, Italy, Nicola Fossati, Lugano, Switzerland, Lucia D’Ambrosio, Milano, Italy, Andrea Gallina, Lugano, Switzerland, Marta Picozzi, Milan, Italy, Manuela Tutolo, Alberto Martini, Milano, Italy, Steven Joniau, Leuven, Belgium, Jeffrey R. Karnes, Rochester, MN, Francesco Montorsi, Alberto Briganti, Milano, Italy

Gabriele Sorce, MD
University of Messina
Poster Presenter(s)
Introduction: The use of 68Ga-PSMA in prostate cancer (PCa) staging is associated with higher nodal specificity and sensitivity as compared to conventional imaging. However, the implications of the introduction of 68Ga-PSMA on oncological outcomes in men with cN1 disease are still unknown.
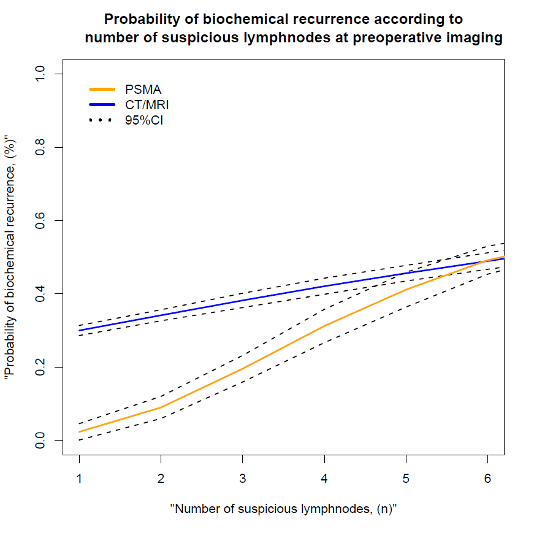
Methods: Overall, 111 patients who underwent radical prostatectomy (RP) with pelvic lymph node dissection (ePLND) for clinically node positive PCa from 2010 to 2021 at three European centers were identified. Preoperative imaging was performed using either conventional imaging (i.e., CT or MRI scan) or PSMA PET/CT. Biochemical recurrence (BCR) was defined as two PSA values =0.2ng/ml. Kaplan-Meier analyses assessed time to BCR. Multivariable Cox-regression analyses tested the impact of imaging modality on BCR after accounting for confounders. A local polynomial smoother weighted function graphically depicted the effect of number of suspicious nodes at imaging with the risk of BCR according to imaging modality.
Results: Median age and PSA was 66 years and 13.8 ng/ml. Overall, 81 patients (73%, Group 1) were staged using conventional (i.e., CT/MRI scan) vs. 30 (27%, Group 2) using PSMA-PET/CT. No baseline differences were reported between the two groups in terms of clinical and biopsy features (all p>0.05). Overall, 56 vs. 70% harboured pN1 disease in Group 1 vs. Group 2. At median follow-up of 32 months, 38 patients had BCR. 12-month BCR was 30% vs. 42% for Group 2 vs. Group 1 (p < 0.01). PSMA PET/CT was associated with lower risk of BCR (HR: 0.3; p=0.02) compared to conventional imaging. The number of suspicious lymphadenopaties was associated with higher risk of BCR (HR: 1.24; p<0.01). The risk of BCR in men with =4 suspicious nodes at imaging was lower for those staged with PSMA PET/CT.
Conclusions: The identification of cN1 disease at 68GaPSMA-PET/CT was associated with lower risk of BCR likely due to better accuracy of this imaging modality in detecting micro-metastatic disease which may allow for the identification of an earlier node positive stage with a better prognosis.
Source of Funding: none
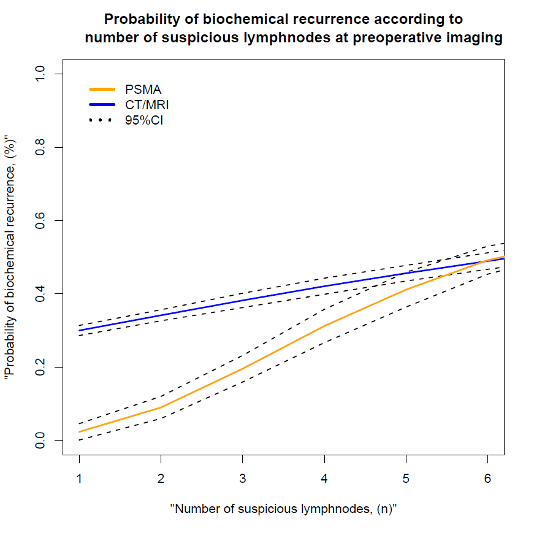
Methods: Overall, 111 patients who underwent radical prostatectomy (RP) with pelvic lymph node dissection (ePLND) for clinically node positive PCa from 2010 to 2021 at three European centers were identified. Preoperative imaging was performed using either conventional imaging (i.e., CT or MRI scan) or PSMA PET/CT. Biochemical recurrence (BCR) was defined as two PSA values =0.2ng/ml. Kaplan-Meier analyses assessed time to BCR. Multivariable Cox-regression analyses tested the impact of imaging modality on BCR after accounting for confounders. A local polynomial smoother weighted function graphically depicted the effect of number of suspicious nodes at imaging with the risk of BCR according to imaging modality.
Results: Median age and PSA was 66 years and 13.8 ng/ml. Overall, 81 patients (73%, Group 1) were staged using conventional (i.e., CT/MRI scan) vs. 30 (27%, Group 2) using PSMA-PET/CT. No baseline differences were reported between the two groups in terms of clinical and biopsy features (all p>0.05). Overall, 56 vs. 70% harboured pN1 disease in Group 1 vs. Group 2. At median follow-up of 32 months, 38 patients had BCR. 12-month BCR was 30% vs. 42% for Group 2 vs. Group 1 (p < 0.01). PSMA PET/CT was associated with lower risk of BCR (HR: 0.3; p=0.02) compared to conventional imaging. The number of suspicious lymphadenopaties was associated with higher risk of BCR (HR: 1.24; p<0.01). The risk of BCR in men with =4 suspicious nodes at imaging was lower for those staged with PSMA PET/CT.
Conclusions: The identification of cN1 disease at 68GaPSMA-PET/CT was associated with lower risk of BCR likely due to better accuracy of this imaging modality in detecting micro-metastatic disease which may allow for the identification of an earlier node positive stage with a better prognosis.
Source of Funding: none

.jpg)
.jpg)