Back
Poster, Podium & Video Sessions
Moderated Poster
MP51: Prostate Cancer: Staging
MP51-19: Pathologic Gleason Grade Group 1 in Black Men Implications for Renaming it "Not Cancer" in High-Risk Populations.
Sunday, May 15, 2022
4:30 PM – 5:45 PM
Location: Room 222
Courtney Berg*, Newark, NJ, Matthew DeMasi, Bronx, NY, Amjad Alwaal, Robert Weiss, Evan Kovac, Newark, NJ
- CB
Courtney Berg, DO
Urology Resident
Rutgers NJMS
Poster Presenter(s)
Introduction: Many have suggested reclassifying Gleason Grade Group 1 (GG1) as “not cancer”. However, the metastatic potential of pathologic (p) GG1 has not been widely studied in high-risk men. Thus, we sought to compare features of pGG1 prostate cancer (PCa) in Black and White men.
Methods: The National Cancer Institute’s Surveillance, Epidemiology and End Results (SEER) database was queried to identify all White and Black men who underwent primary radical prostatectomy (RP) between 2006-2016. Patients were pathologically staged according to the American Joint Committee on Cancer’s 7th edition (2010) and assigned a Gleason score in accordance with the 2005 International Society of Urological Pathology (ISUP) grading system. Only patients with pGG1 PCa and with pelvic lymph node dissections (PLND) were included. Rates of pT3a, pT3b, pT4, pN1 and clinical M+ disease were calculated. Other variables analyzed included prostate-specific antigen (PSA) at diagnosis, age, and year of RP. Nonparametric testing was used to compare differences between White and Black men. Patients with incomplete grading or staging information were excluded.
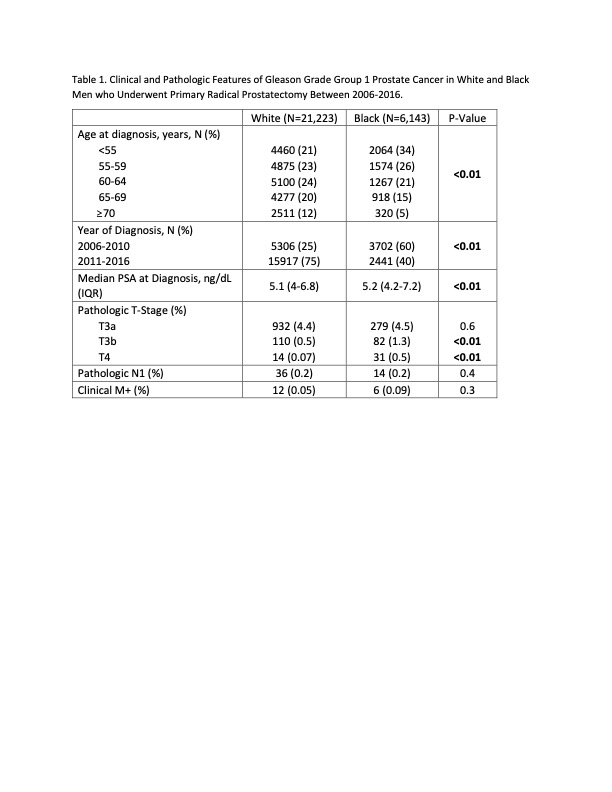
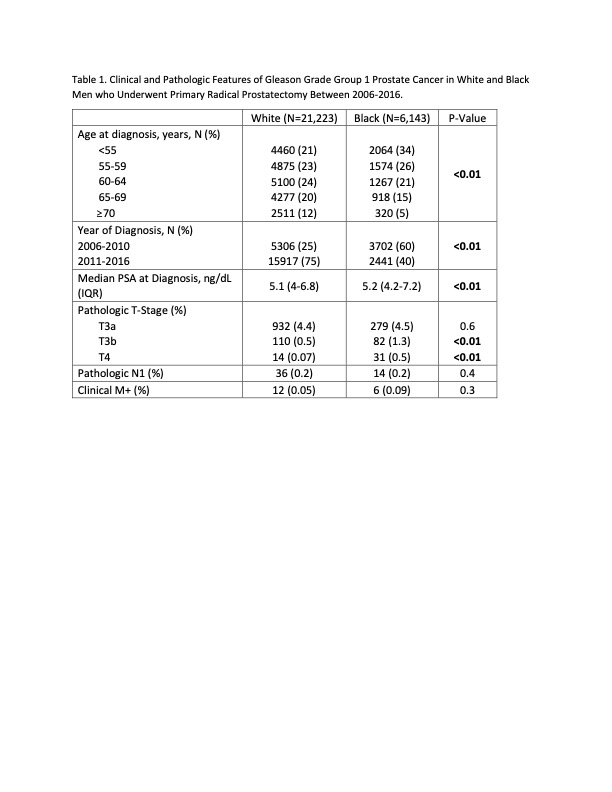
Results: We identified 27,582 White and Black men who underwent RP from 2006-2016 with pGG1 PCa. 216 patients were excluded, leaving 27,367 (21,223 White and 6,143 Black) patients with pGG1 and who underwent PLND in the final analysis (Table 1). Median age range was 60-64 years and 55-59 years for White and Black men, respectively. The median PSA at diagnosis was 5.1 (IQR 4-6.8) and 5.2 (IQR 4.2-7.2) for White and Black men, respectively. Rates of pT3a, pT3b and T4 in White men were 4.4%, 0.5% and 0.07%, respectively, compared to 4.5%, 1.3% and 0.5% for Black men, respectively. Rates of T3b and T4 were statistically higher in Black men (P <0.01 for both). Rates of N1 and M+ were exceedingly low in both groups and were not statistically different.
Conclusions: Black men with pGG1 PCa have low but statistically higher rates of locally advanced disease when compared to White men. Metastatic rates are exceedingly low and similar between the groups. Renaming GG1 to “not cancer” in high-risk populations is therefore controversial. This study is limited by the inability to conduct pathologic and metastatic staging review, especially in cases where under-grading or over-staging are suspected.
Source of Funding: none
Methods: The National Cancer Institute’s Surveillance, Epidemiology and End Results (SEER) database was queried to identify all White and Black men who underwent primary radical prostatectomy (RP) between 2006-2016. Patients were pathologically staged according to the American Joint Committee on Cancer’s 7th edition (2010) and assigned a Gleason score in accordance with the 2005 International Society of Urological Pathology (ISUP) grading system. Only patients with pGG1 PCa and with pelvic lymph node dissections (PLND) were included. Rates of pT3a, pT3b, pT4, pN1 and clinical M+ disease were calculated. Other variables analyzed included prostate-specific antigen (PSA) at diagnosis, age, and year of RP. Nonparametric testing was used to compare differences between White and Black men. Patients with incomplete grading or staging information were excluded.
Results: We identified 27,582 White and Black men who underwent RP from 2006-2016 with pGG1 PCa. 216 patients were excluded, leaving 27,367 (21,223 White and 6,143 Black) patients with pGG1 and who underwent PLND in the final analysis (Table 1). Median age range was 60-64 years and 55-59 years for White and Black men, respectively. The median PSA at diagnosis was 5.1 (IQR 4-6.8) and 5.2 (IQR 4.2-7.2) for White and Black men, respectively. Rates of pT3a, pT3b and T4 in White men were 4.4%, 0.5% and 0.07%, respectively, compared to 4.5%, 1.3% and 0.5% for Black men, respectively. Rates of T3b and T4 were statistically higher in Black men (P <0.01 for both). Rates of N1 and M+ were exceedingly low in both groups and were not statistically different.
Conclusions: Black men with pGG1 PCa have low but statistically higher rates of locally advanced disease when compared to White men. Metastatic rates are exceedingly low and similar between the groups. Renaming GG1 to “not cancer” in high-risk populations is therefore controversial. This study is limited by the inability to conduct pathologic and metastatic staging review, especially in cases where under-grading or over-staging are suspected.
Source of Funding: none

.jpg)
.jpg)