Back
Poster, Podium & Video Sessions
Moderated Poster
MP52: Urodynamics/Lower Urinary Tract Dysfunction/Female Pelvic Medicine: Male Incontinence: Therapy
MP52-05: Pre-existing Detrusor Overactivity Leads To Earlier Artificial Urinary Sphincter Failure and Need for Revision
Monday, May 16, 2022
7:00 AM – 8:15 AM
Location: Room 228
Kevin Krughoff*, Andrew C. Peterson, Durham, NC
Kevin Krughoff, MD
Duke University
Poster Presenter(s)
Introduction: The artificial urinary sphincter (AUS) is the gold standard treatment for post-prostatectomy stress urinary incontinence. While clinical risk factors such as radiation exposure have been evaluated for erosion, bladder mechanics may play an unknown role in device longevity. We hypothesized that poor bladder mechanics such as detrusor overactivity (DO) are associated with the need for earlier surgical device revision.
Methods: A prospectively maintained, IRB approved institutional database was queried for CPT codes 53445-53449 spanning years 1997-2021. 2,243 encounters comprising 524 unique patient records were individually reviewed. Records with primary AUS removal or replacement, history of radical prostatectomy, baseline urodynamic study (UDS), voiding diary and pad weights were included for analysis. Results from cystoscopy and pelvic x-ray of the contrast-filled devices were reviewed to assess failure etiology. Multiple imputation of chained equations was performed for missing data elements. Variables with significant correlation on univariate analysis or strong theoretical association with AUS longevity were entered for Cox proportional hazards modeling. Partial correlation coefficients between variables were assessed for collinearity.
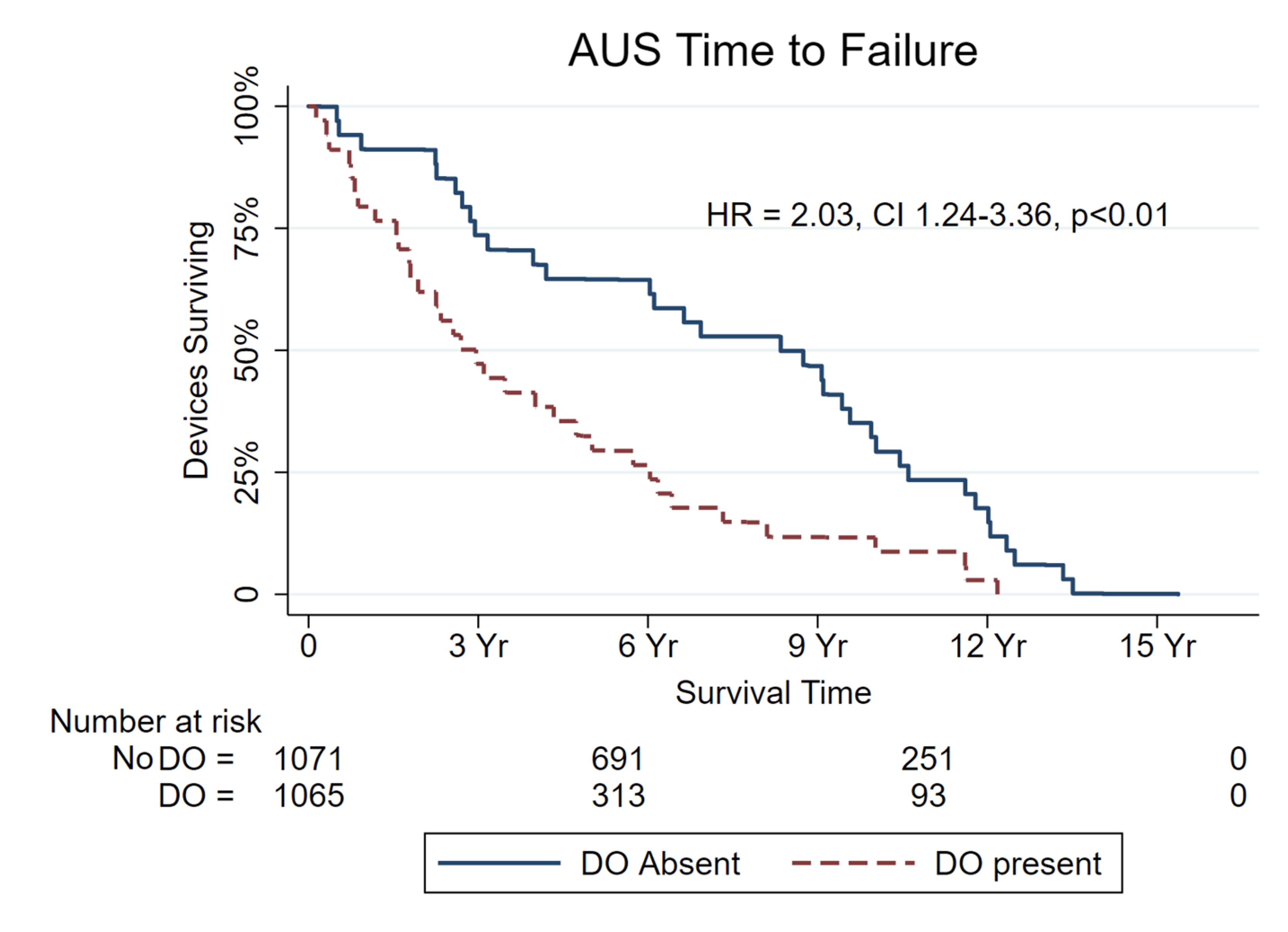
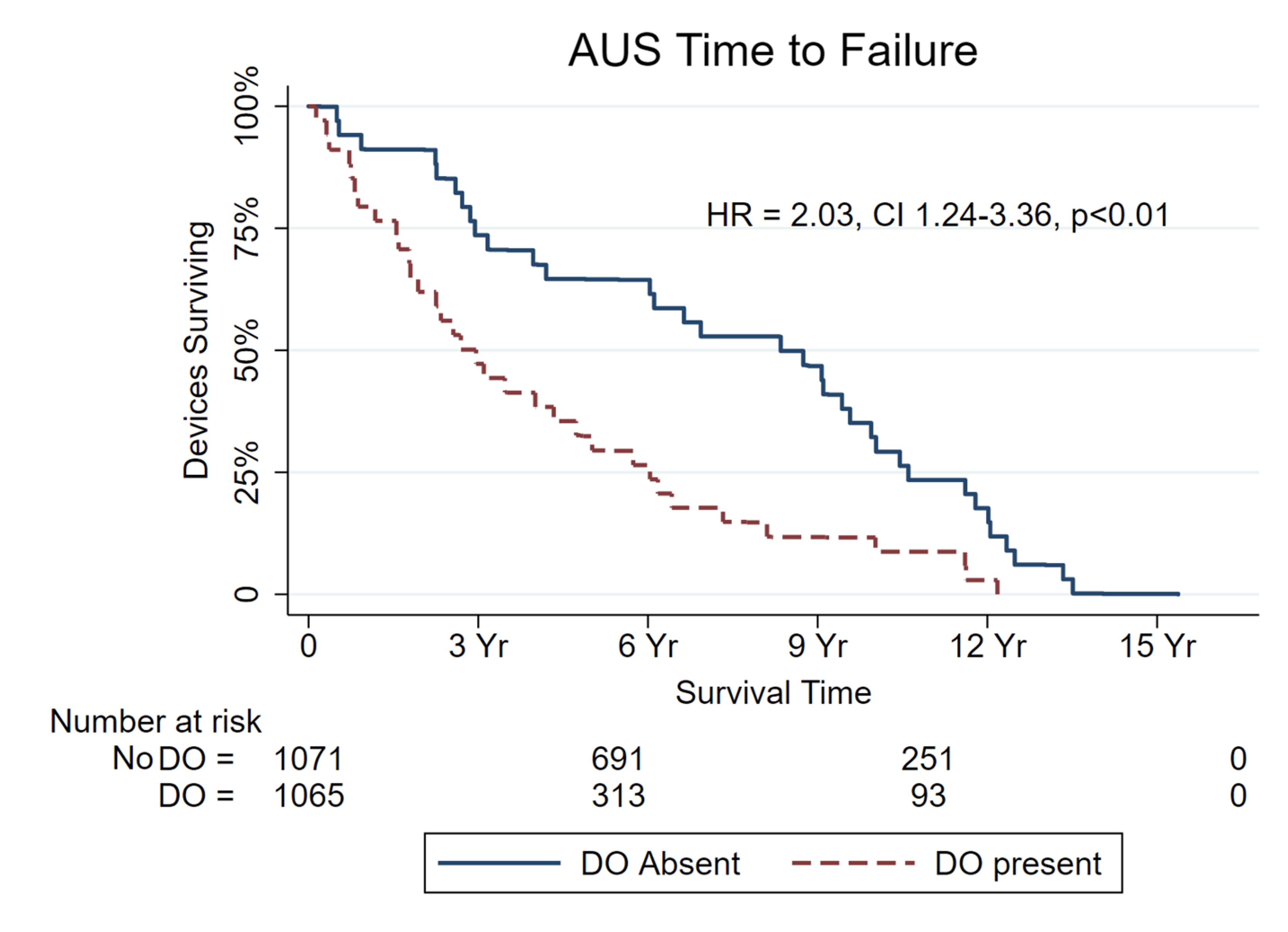
Results: Ninety-two records met criteria for analysis. The median time to intervention was 2070 days (823, 3442). Intervention was prompted by mechanical failure (41.8%), sub-cuff atrophy (38.8%), erosion (9.0%), infection (8.8%) or patient preference (1.5%). AUS longevity was associated with age (p=0.01), volume at strong sensation (p < 0.01), capacity (p < 0.01) and DO (p < 0.01). On multivariate analysis, DO was significantly associated with time to intervention (HR = 2.03; 95% CI 1.24 – 3.36; p<0.01) when controlling for radiation history, BMI, diabetes and smoking status. No other clinical variables were associated with AUS longevity.
Conclusions: In men with uncomplicated post-prostatectomy incontinence, the intervention rate for AUS removal or replacement is twice as high in men with pre-existing DO. Clinical characteristics typically related to tissue quality and healing potential were not significantly related to device longevity when accounting for bladder dynamics.
Source of Funding: Boston Scientific Fellowship Grant
Methods: A prospectively maintained, IRB approved institutional database was queried for CPT codes 53445-53449 spanning years 1997-2021. 2,243 encounters comprising 524 unique patient records were individually reviewed. Records with primary AUS removal or replacement, history of radical prostatectomy, baseline urodynamic study (UDS), voiding diary and pad weights were included for analysis. Results from cystoscopy and pelvic x-ray of the contrast-filled devices were reviewed to assess failure etiology. Multiple imputation of chained equations was performed for missing data elements. Variables with significant correlation on univariate analysis or strong theoretical association with AUS longevity were entered for Cox proportional hazards modeling. Partial correlation coefficients between variables were assessed for collinearity.
Results: Ninety-two records met criteria for analysis. The median time to intervention was 2070 days (823, 3442). Intervention was prompted by mechanical failure (41.8%), sub-cuff atrophy (38.8%), erosion (9.0%), infection (8.8%) or patient preference (1.5%). AUS longevity was associated with age (p=0.01), volume at strong sensation (p < 0.01), capacity (p < 0.01) and DO (p < 0.01). On multivariate analysis, DO was significantly associated with time to intervention (HR = 2.03; 95% CI 1.24 – 3.36; p<0.01) when controlling for radiation history, BMI, diabetes and smoking status. No other clinical variables were associated with AUS longevity.
Conclusions: In men with uncomplicated post-prostatectomy incontinence, the intervention rate for AUS removal or replacement is twice as high in men with pre-existing DO. Clinical characteristics typically related to tissue quality and healing potential were not significantly related to device longevity when accounting for bladder dynamics.
Source of Funding: Boston Scientific Fellowship Grant

.jpg)
.jpg)