Back
Poster, Podium & Video Sessions
Moderated Poster
MP52: Urodynamics/Lower Urinary Tract Dysfunction/Female Pelvic Medicine: Male Incontinence: Therapy
MP52-07: Impact of Frailty on Adverse Complications Following Artificial Urinary Sphincter Implantation
Monday, May 16, 2022
7:00 AM – 8:15 AM
Location: Room 228
Rohan Bhalla*, Jackson Cabo, Tanya Marvi, Abimbola Ayangbesan, George Koch, Stephen Hill, Douglas Milam, Melissa Kaufman, Niels Johnsen, Nashville, TN

Rohan G. Bhalla, MD
Vanderbilt University Medical Center
Poster Presenter(s)
Introduction: Frailty is a well-established predictor of postoperative outcomes. We aimed to investigate the association between the modified Frailty Index (mFI) and postoperative complications after artificial urinary sphincter (AUS) surgery.
Methods: Men who underwent AUS surgery at a single institution (1/1/13 – 7/31/2020) were identified and electronic medical records were reviewed. The mFI is a validated measure of predicting patient morbidity and mortality that consists of 11 patient co-morbidities. Each variable is given 1 point with composite scores ranging from 0 (no frailty) to 11 (highest degree of frailty). Operative and non-operative complications were categorized as: mechanical failure, cuff erosion, infection, intractable pain, urinary retention, or other. Multivariable logistic regression was used to identify an association between mFI and postoperative complications.
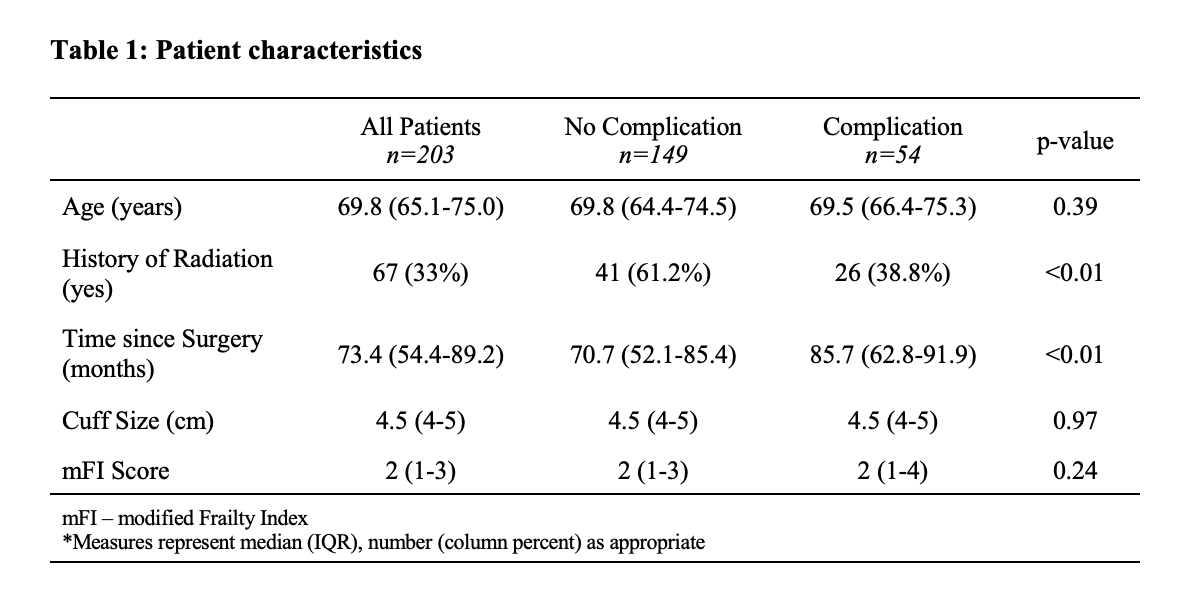
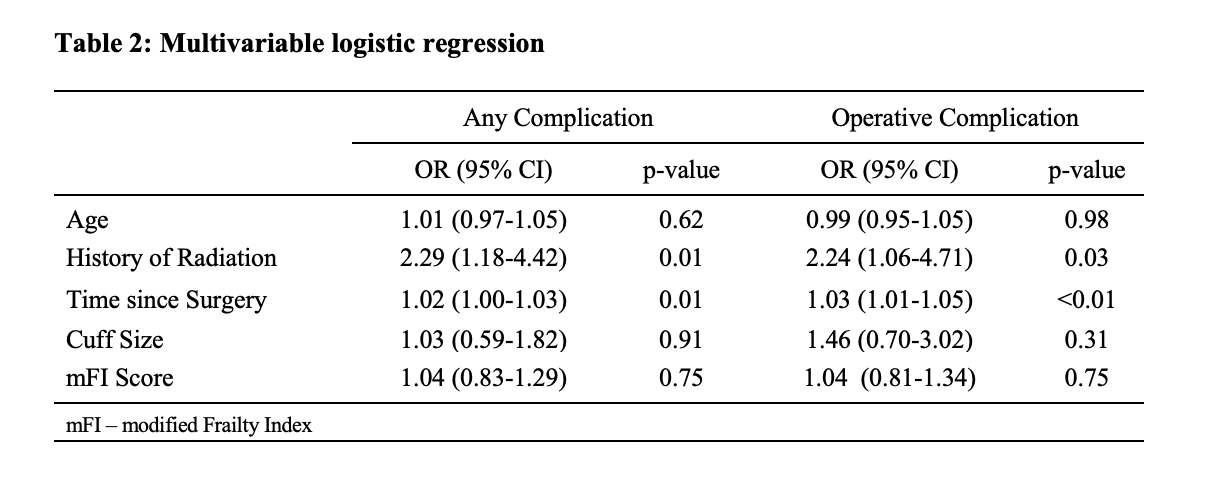
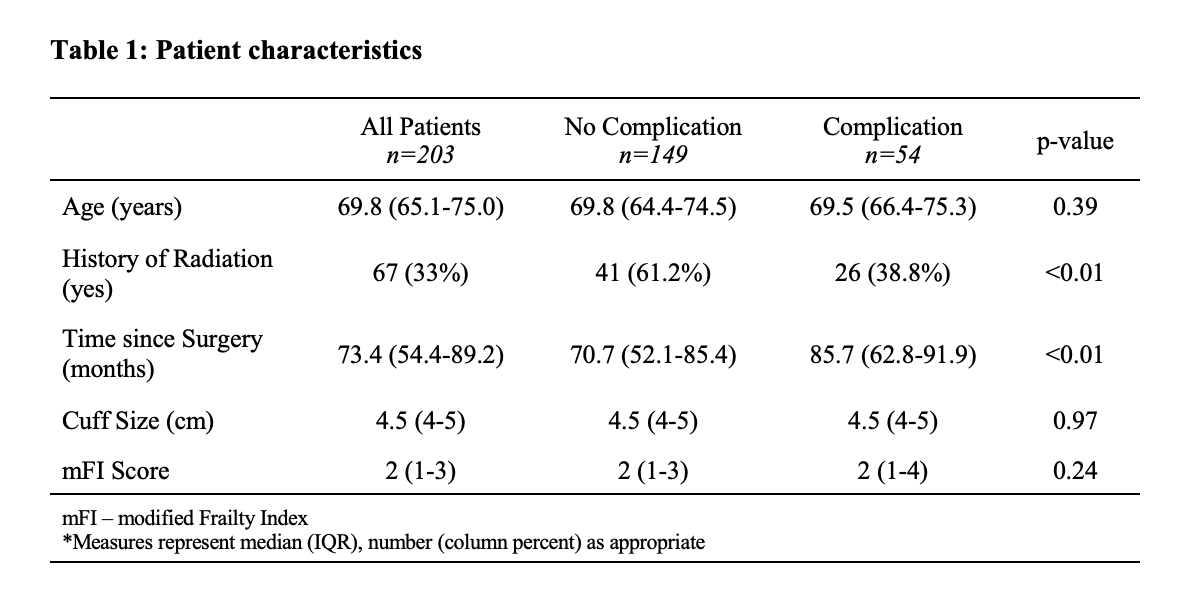
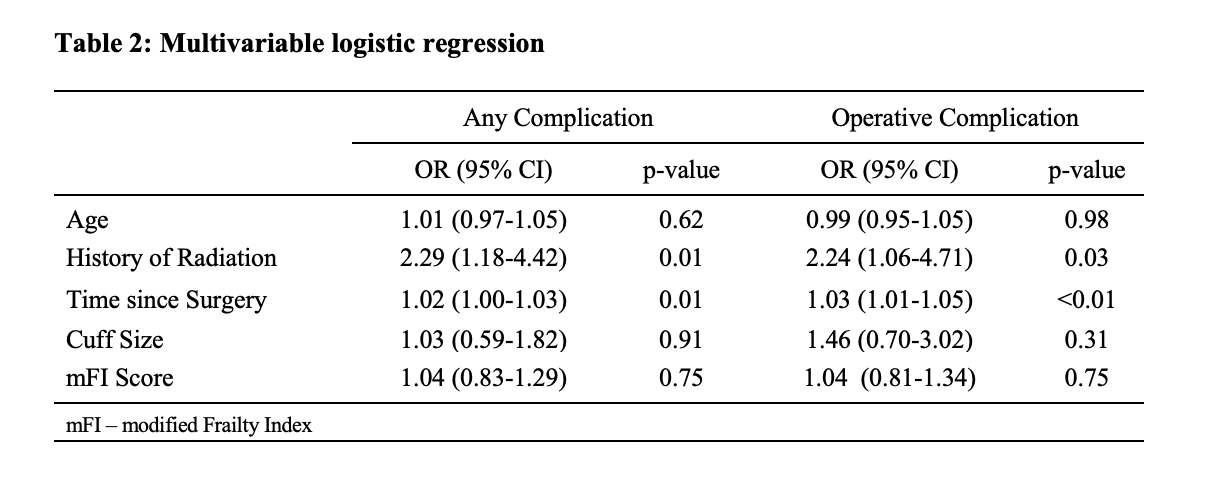
Results: 203 AUS patients met inclusion criteria. The median age was 69.8 years (IQR 65.1-75.0) with 33% (n=67) of patients having a history of radiation and 29.1% (n=59) of patients with a history of diabetes mellitus. The median time from surgery to data collection was 73.4 months (IQR 54.4-89.2). The median cuff size was 4.5cm (IQR 4-5). The complication rate was 26.6% with 18.7% of men requiring a surgical intervention (mechanical failure: n=11, cuff erosion: n=16, infection: n=7, other n=4). The median mFI was 2 (IQR 1-4) for patients with a complication and 2 (IQR 1-3) for those with no complication (Table 1). Multivariable analysis demonstrated no association between mFI and overall complication (OR 1.04, 95% CI 0.83-1.29; p=0.75) or surgical complication (OR 1.04, 95% CI 0.81-1.34; p=0.75). Prior radiation and time since surgery were significantly associated with postoperative complications (Table 2).
Conclusions: The mFI was not associated with an increased risk of AUS complications. However, a prior history of radiation and extended time from surgery were independently associated with complications and the need for surgical intervention.
Source of Funding: N/a
Methods: Men who underwent AUS surgery at a single institution (1/1/13 – 7/31/2020) were identified and electronic medical records were reviewed. The mFI is a validated measure of predicting patient morbidity and mortality that consists of 11 patient co-morbidities. Each variable is given 1 point with composite scores ranging from 0 (no frailty) to 11 (highest degree of frailty). Operative and non-operative complications were categorized as: mechanical failure, cuff erosion, infection, intractable pain, urinary retention, or other. Multivariable logistic regression was used to identify an association between mFI and postoperative complications.
Results: 203 AUS patients met inclusion criteria. The median age was 69.8 years (IQR 65.1-75.0) with 33% (n=67) of patients having a history of radiation and 29.1% (n=59) of patients with a history of diabetes mellitus. The median time from surgery to data collection was 73.4 months (IQR 54.4-89.2). The median cuff size was 4.5cm (IQR 4-5). The complication rate was 26.6% with 18.7% of men requiring a surgical intervention (mechanical failure: n=11, cuff erosion: n=16, infection: n=7, other n=4). The median mFI was 2 (IQR 1-4) for patients with a complication and 2 (IQR 1-3) for those with no complication (Table 1). Multivariable analysis demonstrated no association between mFI and overall complication (OR 1.04, 95% CI 0.83-1.29; p=0.75) or surgical complication (OR 1.04, 95% CI 0.81-1.34; p=0.75). Prior radiation and time since surgery were significantly associated with postoperative complications (Table 2).
Conclusions: The mFI was not associated with an increased risk of AUS complications. However, a prior history of radiation and extended time from surgery were independently associated with complications and the need for surgical intervention.
Source of Funding: N/a

.jpg)
.jpg)