Back
Poster, Podium & Video Sessions
Moderated Poster
MP52: Urodynamics/Lower Urinary Tract Dysfunction/Female Pelvic Medicine: Male Incontinence: Therapy
MP52-11: Bladder Neck Contractures Stabilize after Artificial Urinary Sphincter Placement
Monday, May 16, 2022
7:00 AM – 8:15 AM
Location: Room 228
Kevin Krughoff*, Hayley Premo, Andrew C. Peterson, Durham, NC
Kevin Krughoff, MD
Duke University
Poster Presenter(s)
Introduction: The optimal treatment for the combination of stress urinary incontinence (SUI) and bladder neck contracture (BNC) is often vexing to the reconstructive urologist. Anecdotal clinical experience from our group indicates that many BNCs stabilize after AUS placement. We hypothesize that AUS placement may decrease BNC recurrence.
Methods: Men with BNC and voiding LUTS or AUR are treated at our institution with dilation, DVIU or TUR. Men with SUI electing AUS placement undergo simultaneous BNC treatment if symptomatic or if the bladder neck is = 12 French and precludes catheter insertion. We queried our prospectively maintained QI database for all patients seen at our institution from 2001-2021 with a history of SUI and intervention for BNC. A total of 174 records were reviewed. Those with a urethral stent (n=6) or less than 2 months follow up (n=9) were excluded. The odds of recurrence and time between recurrences were compared between those with and without an AUS in place using logistic regression and the Wilcoxon Rank-Sum test. Recurrence rates and recurrence free survival were compared using multivariate Cox regression.
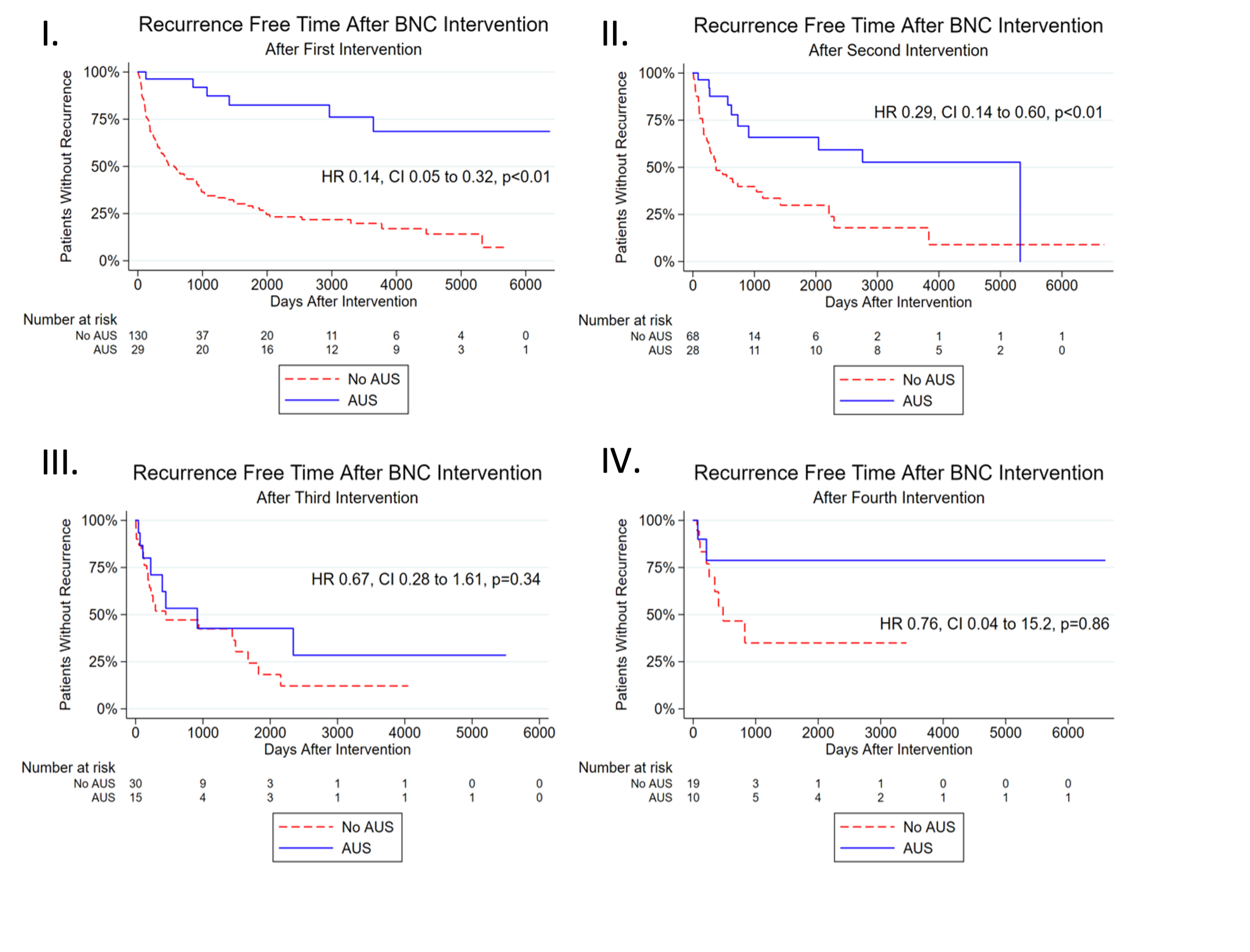
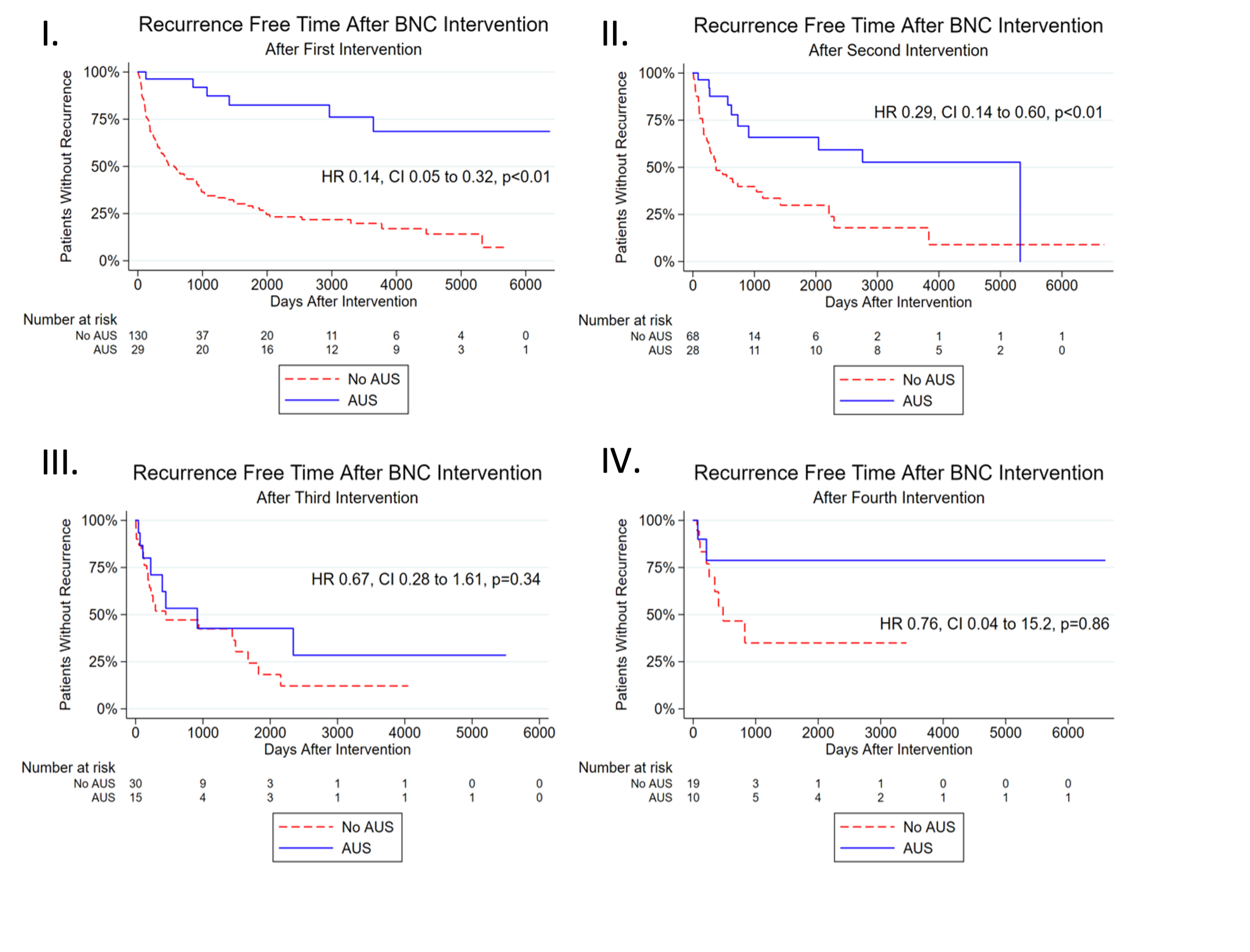
Results: The analytic cohort of 159 was comprised of 60 patients who underwent AUS placement and 99 who did not. Baseline characteristics were similar except for a 15% higher prevalence of pelvic radiation in the AUS group (p=0.06). A total of 278 BNC interventions were carried out in the non-AUS group (median 2 per patient) and 83 in the AUS group (median 2 per patient). After any given BNC intervention, the odds of recurrence were 75% lower (OR 0.25, CI: 0.15-0.42, p<0.01) when an AUS was placed. On sub-analysis according to number of prior interventions, AUS placement was associated with a 90% lower odds of recurrence (OR 0.10, CI: 0.03-0.27, p<0.01) and 2.6 years (p=0.02) longer time to recurrence after one intervention. After two interventions, the odds were 61% less (OR 0.39, CI: 0.16-0.97, p=0.04) and time to recurrence was 1.3 years longer (p=0.01). Recurrence rates were 70% and 75% lower at these same time points when adjusting for prior radiation, prostatectomy, receipt of CIC teaching, smoking, age, diabetes and coronary artery disease (Figure 1).
Conclusions: Our data indicate that placement of the AUS seems to be associated with improved bladder neck stability.
Source of Funding: Boston Scientific Fellowship Grant
Methods: Men with BNC and voiding LUTS or AUR are treated at our institution with dilation, DVIU or TUR. Men with SUI electing AUS placement undergo simultaneous BNC treatment if symptomatic or if the bladder neck is = 12 French and precludes catheter insertion. We queried our prospectively maintained QI database for all patients seen at our institution from 2001-2021 with a history of SUI and intervention for BNC. A total of 174 records were reviewed. Those with a urethral stent (n=6) or less than 2 months follow up (n=9) were excluded. The odds of recurrence and time between recurrences were compared between those with and without an AUS in place using logistic regression and the Wilcoxon Rank-Sum test. Recurrence rates and recurrence free survival were compared using multivariate Cox regression.
Results: The analytic cohort of 159 was comprised of 60 patients who underwent AUS placement and 99 who did not. Baseline characteristics were similar except for a 15% higher prevalence of pelvic radiation in the AUS group (p=0.06). A total of 278 BNC interventions were carried out in the non-AUS group (median 2 per patient) and 83 in the AUS group (median 2 per patient). After any given BNC intervention, the odds of recurrence were 75% lower (OR 0.25, CI: 0.15-0.42, p<0.01) when an AUS was placed. On sub-analysis according to number of prior interventions, AUS placement was associated with a 90% lower odds of recurrence (OR 0.10, CI: 0.03-0.27, p<0.01) and 2.6 years (p=0.02) longer time to recurrence after one intervention. After two interventions, the odds were 61% less (OR 0.39, CI: 0.16-0.97, p=0.04) and time to recurrence was 1.3 years longer (p=0.01). Recurrence rates were 70% and 75% lower at these same time points when adjusting for prior radiation, prostatectomy, receipt of CIC teaching, smoking, age, diabetes and coronary artery disease (Figure 1).
Conclusions: Our data indicate that placement of the AUS seems to be associated with improved bladder neck stability.
Source of Funding: Boston Scientific Fellowship Grant

.jpg)
.jpg)