Back
Poster, Podium & Video Sessions
Moderated Poster
MP53: Prostate Cancer: Detection & Screening V
MP53-02: Comparison of Highest-grade Tumor Percentage in Core Samples from MRI-targeted Biopsy and Systematic Biopsy for Prostate Cancer Diagnosis
Monday, May 16, 2022
7:00 AM – 8:15 AM
Location: Room 225
Shu Wang*, Ryan Russell, Ashley Park, Alexa Van Besien, Adrianna Lee, Linhan Xu, Ankur Choksi, M. Adil Afzal, Amelia Wnorowski, Michael Naslund, M. Minhaj Siddiqui, Baltimore, MD

Shu Wang, MD
University of Maryland School of Medicine
Poster Presenter(s)
Introduction: The advent of magnetic resonance imaging (MRI)-targeted biopsy (TB) has allowed for higher rate of detection of clinically significant prostate cancers (CSPCa) than systematic biopsy (SB). However, it remains to be demonstrated if the improved targeting also leads to more accurate representation of tumor volume by sampling the center, rather than periphery, of the tumor nodule. This study aims to compare the two biopsy methods in its ability to detect a higher percentage of the highest-grade tumor in core samples.
Methods: We retrospectively reviewed patients who underwent both MRI-TB and SB of prostate from 2015 to 2020. Patients with a history of PCa were removed from the study cohort. The core samples with the highest Gleason scores (GS) were isolated for each biopsy method, followed by identification of the corresponding maximum percentage tumor. CSPCa was defined as GS>6. T-test was performed to compare the maximum tumor percentages from biopsy cores between TB and SB.
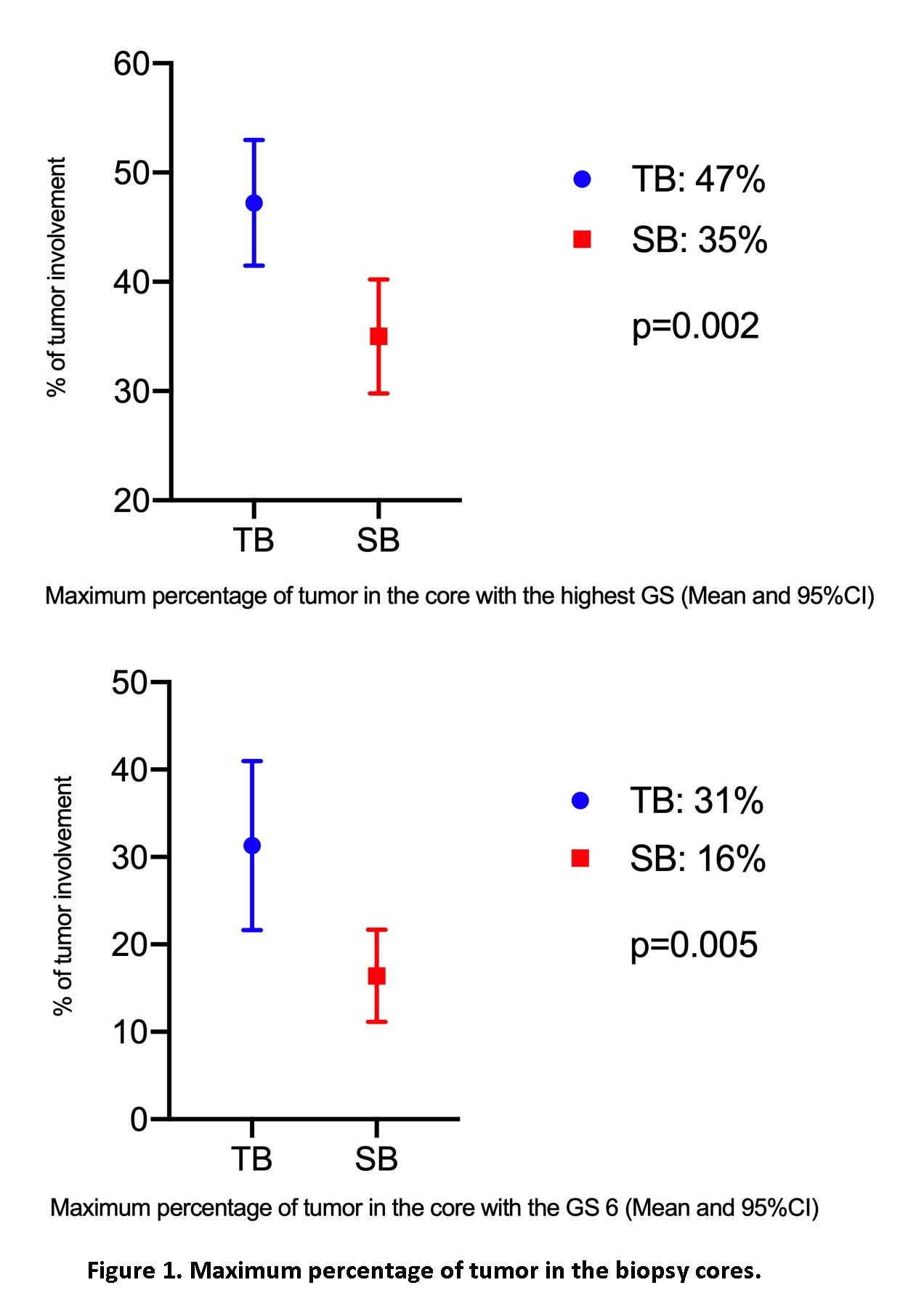
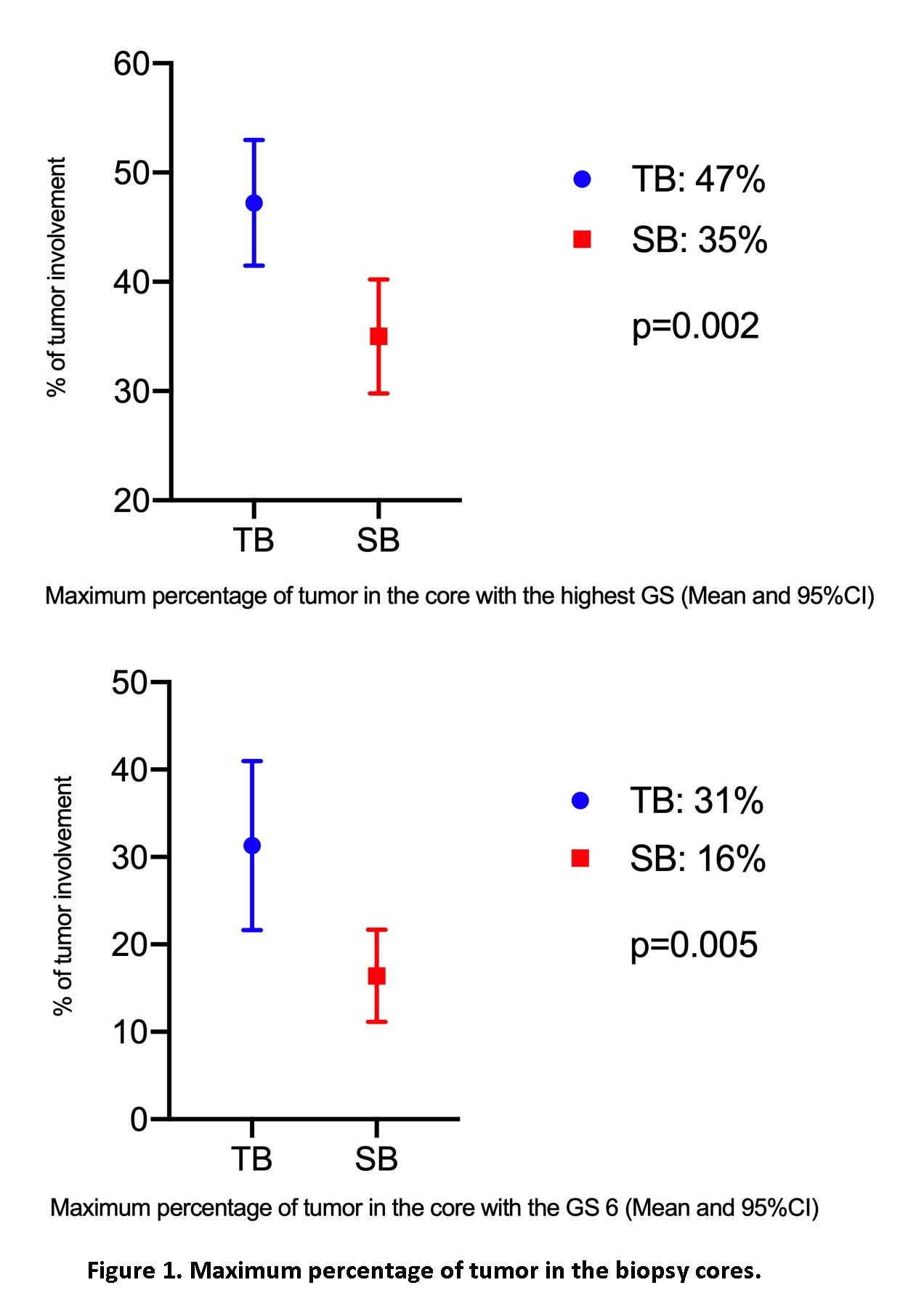
Results: 297 patients were identified. Those with benign biopsy results for both TB and SB and no available information on biopsy cores were excluded, resulting in 148 (49.8%) patients for analysis. Mean age was 64 years. Races included 60.8% (90/148) Caucasians and 29.7% (44/148) African Americans. Mean PSA level was 10.3ng/ml. 48.6% (72/148) patients had a previous negative biopsy. CSPCas were found in 72.3% (107/148) for combined TB/SB vs 59.5% (88/148) on TB vs 55.4% (82/148) on SB. Overall, the mean maximum percentage of tumor in the core with the highest GS was higher for TB vs SB (47% vs 35%, p=0.002). When examining GS>6 lesions, the maximum percentages of tumor in the core were 53.7% on TB vs 45.0% on SB (p=0.067), while for GS 6 lesions, the maximum percentages of tumor in the core were 31.3% on TB vs 16.4% on SB (p=0.005) (Figure 1).
Conclusions: In men that underwent both MRI-TB and SB, the TB demonstrated higher percentage of tumor in the biopsy core. This information should be considered when integrating TB data into existing risk-stratification methods and decision-making.
Source of Funding: None.
Methods: We retrospectively reviewed patients who underwent both MRI-TB and SB of prostate from 2015 to 2020. Patients with a history of PCa were removed from the study cohort. The core samples with the highest Gleason scores (GS) were isolated for each biopsy method, followed by identification of the corresponding maximum percentage tumor. CSPCa was defined as GS>6. T-test was performed to compare the maximum tumor percentages from biopsy cores between TB and SB.
Results: 297 patients were identified. Those with benign biopsy results for both TB and SB and no available information on biopsy cores were excluded, resulting in 148 (49.8%) patients for analysis. Mean age was 64 years. Races included 60.8% (90/148) Caucasians and 29.7% (44/148) African Americans. Mean PSA level was 10.3ng/ml. 48.6% (72/148) patients had a previous negative biopsy. CSPCas were found in 72.3% (107/148) for combined TB/SB vs 59.5% (88/148) on TB vs 55.4% (82/148) on SB. Overall, the mean maximum percentage of tumor in the core with the highest GS was higher for TB vs SB (47% vs 35%, p=0.002). When examining GS>6 lesions, the maximum percentages of tumor in the core were 53.7% on TB vs 45.0% on SB (p=0.067), while for GS 6 lesions, the maximum percentages of tumor in the core were 31.3% on TB vs 16.4% on SB (p=0.005) (Figure 1).
Conclusions: In men that underwent both MRI-TB and SB, the TB demonstrated higher percentage of tumor in the biopsy core. This information should be considered when integrating TB data into existing risk-stratification methods and decision-making.
Source of Funding: None.

.jpg)
.jpg)