Back
Poster, Podium & Video Sessions
Moderated Poster
MP53: Prostate Cancer: Detection & Screening V
MP53-08: Effect of Nearness to Cancer Centre on Prostate Cancer Outcomes and Patient&[prime]s Choice for The Type of Intervention
Monday, May 16, 2022
7:00 AM – 8:15 AM
Location: Room 225
Waleed Shabana, Vahid Mehrnoush*, Neda Ghaffari-Marandi, Kristi Dolcetti, Hazem Elmansy, Kevin Ramchandar, Edwin Long, Ahmed Zakaria, Ahmed Kotb, Walid Shahrour, Thunder Bay, Canada
- VM
Vahid Mehrnoush, MD,MSC
Northern Ontario School of Medicine University
Poster Presenter(s)
Introduction: Accessibility to the cancer centre and the urology service may be crucial in the diagnosis and management of prostate cancer while in curable stage. All urology referrals are sent to our tertiary care centre that covers an area of 526,000 square kilometers. We aim to investigate the relationship between nearness to treatment centre to presentation and treatment choice.
Methods: A cohort of 959 patients who diagnosed as prostate cancer between 2010 and 2017 were retrospectively reviewed. The baseline demographics, postal code, round trip time to cancer centre, availability of, clinical staging, PSA at diagnosis, pathological data at biopsy, staging investigations, selected treatment option and its follow up data were reported. Urology, radiation oncology and medical oncology services are only available in our centre. The cohort was split into two groups above and below 300Km depending on distance from our centre due to geographical distribution of our patients. The correlation between distance from patient location to the hospital and clinical stage, Gleason score, PSA, pathological staging, and selected treatment modality were statistically analyzed.
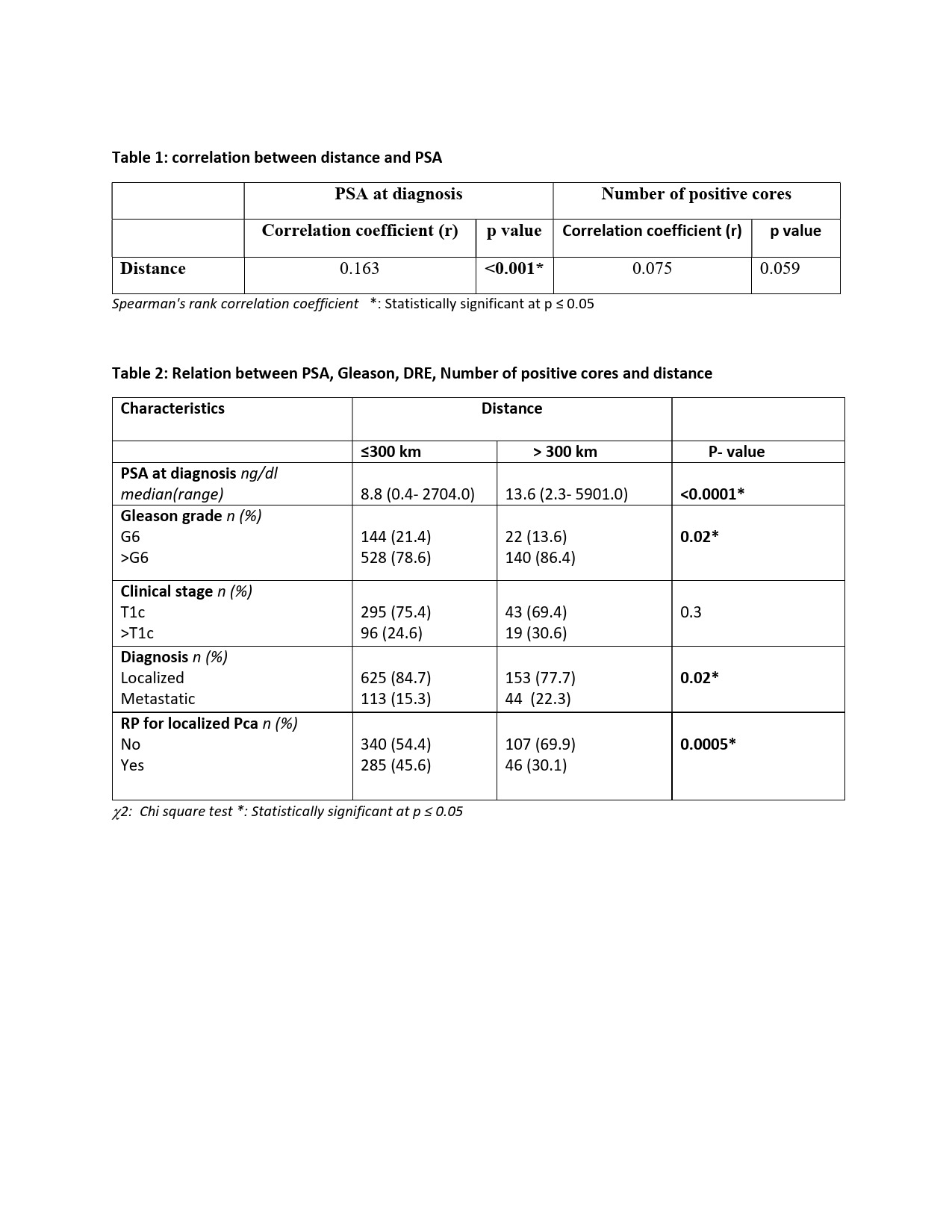
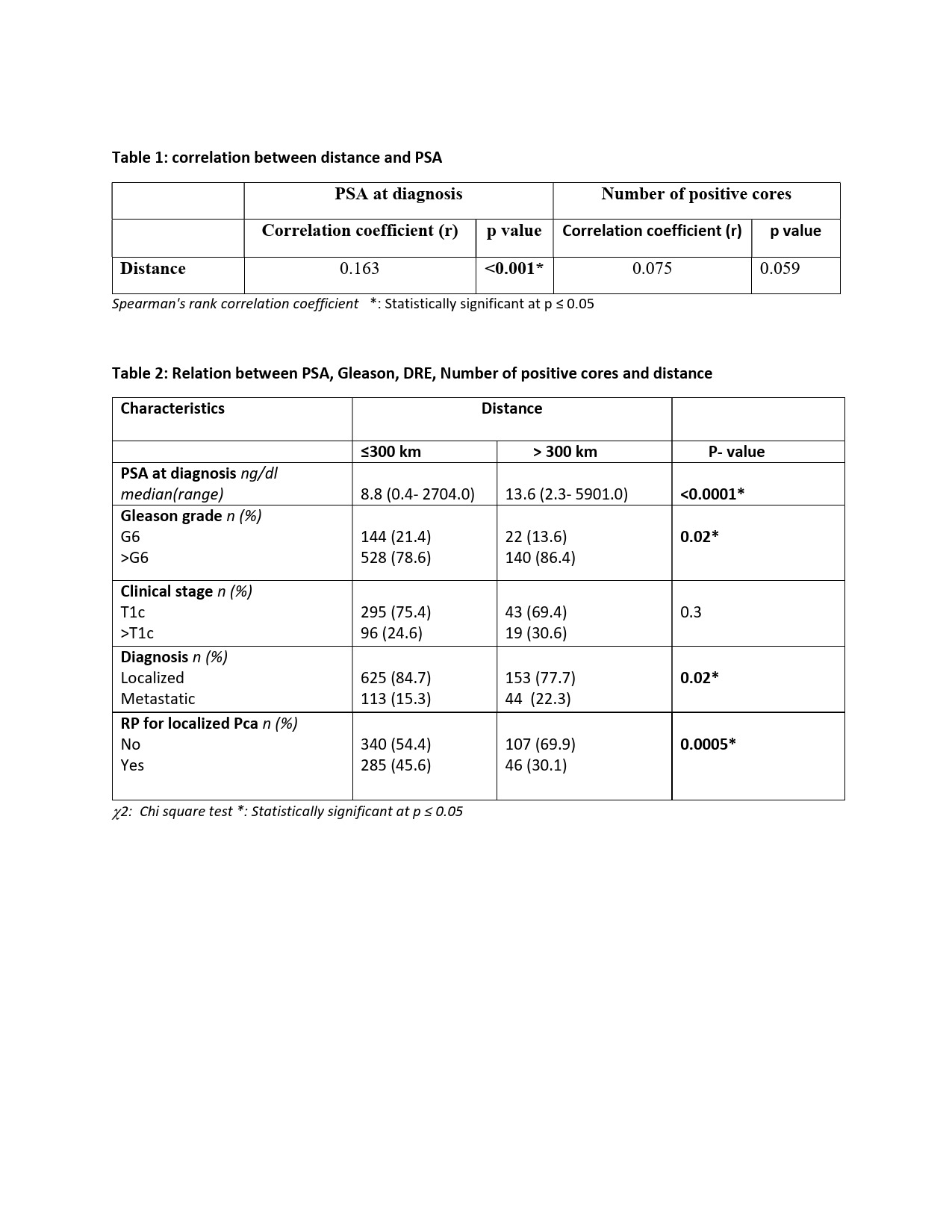
Results: The mean distance from patient residence to hospital was 115.7 Km. There was a significant correlation between PSA at diagnosis and distance to the hospital (p <0.001, Correlation coefficient= 0.16). The median PSA at diagnosis was 8.8 ng/dl Vs 13.6 ng/dl between patient group =300 Km compared to patient group >300KM. The percentage of Gleason 6 patients was significantly lower in the group that lived >300Km (13.6% Vs 21.4% P=0.002). The initial diagnosis of metastatic prostate cancer was found to be significantly higher in the group that lived > 300 Km from treatment centre (22.3% Vs 15.3% P=0.02). The choice of radical prostatectomy as a treatment modality was found to be significantly higher in the group that lived >300Km away from treatment centre (69.9% Vs 54.4% P= 0.0005).
Conclusions: Distance from urologists and cancer centre plays a significant role in the presentation and treatment of prostate cancer. PSA was found to increase for every Km the patient is away from the urologist. Distance was a factor in the choice of radical prostatectomy compared to radiation likely secondary to the reduction in travelling.
Source of Funding: None
Methods: A cohort of 959 patients who diagnosed as prostate cancer between 2010 and 2017 were retrospectively reviewed. The baseline demographics, postal code, round trip time to cancer centre, availability of, clinical staging, PSA at diagnosis, pathological data at biopsy, staging investigations, selected treatment option and its follow up data were reported. Urology, radiation oncology and medical oncology services are only available in our centre. The cohort was split into two groups above and below 300Km depending on distance from our centre due to geographical distribution of our patients. The correlation between distance from patient location to the hospital and clinical stage, Gleason score, PSA, pathological staging, and selected treatment modality were statistically analyzed.
Results: The mean distance from patient residence to hospital was 115.7 Km. There was a significant correlation between PSA at diagnosis and distance to the hospital (p <0.001, Correlation coefficient= 0.16). The median PSA at diagnosis was 8.8 ng/dl Vs 13.6 ng/dl between patient group =300 Km compared to patient group >300KM. The percentage of Gleason 6 patients was significantly lower in the group that lived >300Km (13.6% Vs 21.4% P=0.002). The initial diagnosis of metastatic prostate cancer was found to be significantly higher in the group that lived > 300 Km from treatment centre (22.3% Vs 15.3% P=0.02). The choice of radical prostatectomy as a treatment modality was found to be significantly higher in the group that lived >300Km away from treatment centre (69.9% Vs 54.4% P= 0.0005).
Conclusions: Distance from urologists and cancer centre plays a significant role in the presentation and treatment of prostate cancer. PSA was found to increase for every Km the patient is away from the urologist. Distance was a factor in the choice of radical prostatectomy compared to radiation likely secondary to the reduction in travelling.
Source of Funding: None

.jpg)
.jpg)