Back
Poster, Podium & Video Sessions
Moderated Poster
MP54: Bladder Cancer: Non-invasive II
MP54-08: Urinary comprehensive genomic profiling predicts clinical recurrence in patients undergoing surveillance for urothelial carcinoma
Monday, May 16, 2022
8:45 AM – 10:00 AM
Location: Room 228
Jason Lee, Boston, MA, Vincent Bicocca, Vincent Caruso, Brian Mazzarella, Kevin Phillips, Trevor Levin, San Francisco, CA, Adam Feldman, Keyan Salari*, Boston, MA
- KS
Poster Presenter(s)
Introduction: Risk stratification of patients with urothelial carcinoma (UC) remains a major clinical challenge, with high rates of recurrence and disease progression. Urinary comprehensive genomic profiling (uCGP) has significant potential to aid in this endeavor.
Methods: uCGP was performed on blinded urine specimens collected at Massachusetts General Hospital prior to cystoscopy. 41 subjects with a history of UC but negative by surveillance cystoscopy at time of collection were analyzed. Urine DNA was sequenced and comprehensively profiled across 60 genes using the CLIA-validated UroAmplitude test (Convergent Genomics). Patients were predicted to be at high or low risk of recurrence using a machine learning algorithm based on genomic features. Cox proportional hazards models were used to estimate the association between risk predictions and recurrence-free survival.
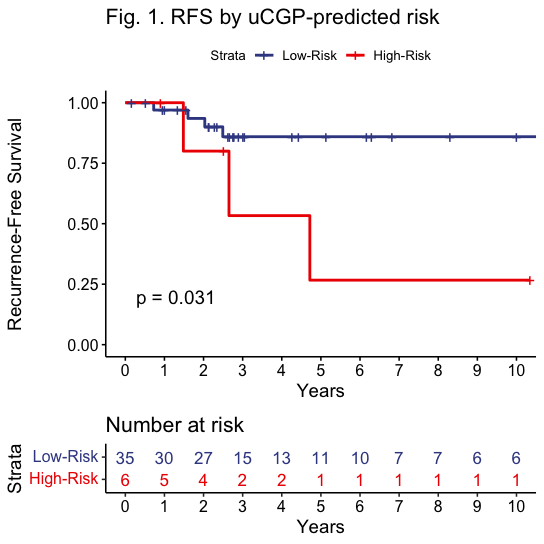
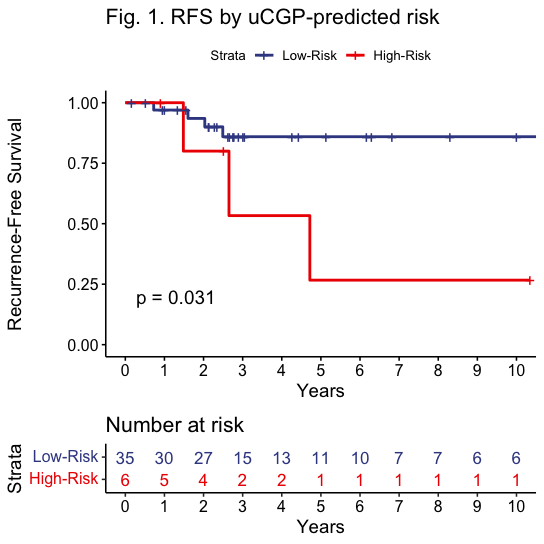
Results: Stage and grade distribution of the primary tumor at diagnosis was Ta (73%), T1 (22%), T3 (2%), Tx (2%), with concomitant CIS in 10%; 41% low-grade (LG) and 59% high-grade (HG). Mean follow-up since specimen collection was 53.3 months. High recurrence risk was predicted in 15% (6 of 41) of subjects who had a positive UroAmplitude disease classification but negative cystoscopy. Among predicted high-risk patients, 50% had a clinical recurrence (mean time to recurrence 35.3 mo), all of which were HG. One notable high-risk patient with an initial TaLG tumor experienced a T4aHG recurrence with invasion into the prostate. uGCP-based recurrence prediction anticipated this clinical diagnosis by 17.8 months. Among 35 predicted low-risk patients, only 4 experienced recurrence (all TaLG; mean time to recurrence 20.5 mo). Recurrence-free survival was significantly worse in uGCP-predicted high-risk vs. low-risk patients (HR 4.5, 95% CI 1.01-20.2; Fig. 1). Among 10 subjects with no detectable mutations, no pathologically confirmed recurrence was observed (mean surveillance follow-up 45.3 mo).
Conclusions: uCGP can predict future recurrence of high-risk UC with substantial lead time. If validated with further studies, uCGP may provide a powerful way to risk-stratify patients and enable strategies for intensification (or deintensification) of UC management based on genomic risk.
Source of Funding: Convergent Genomics, Inc.
Methods: uCGP was performed on blinded urine specimens collected at Massachusetts General Hospital prior to cystoscopy. 41 subjects with a history of UC but negative by surveillance cystoscopy at time of collection were analyzed. Urine DNA was sequenced and comprehensively profiled across 60 genes using the CLIA-validated UroAmplitude test (Convergent Genomics). Patients were predicted to be at high or low risk of recurrence using a machine learning algorithm based on genomic features. Cox proportional hazards models were used to estimate the association between risk predictions and recurrence-free survival.
Results: Stage and grade distribution of the primary tumor at diagnosis was Ta (73%), T1 (22%), T3 (2%), Tx (2%), with concomitant CIS in 10%; 41% low-grade (LG) and 59% high-grade (HG). Mean follow-up since specimen collection was 53.3 months. High recurrence risk was predicted in 15% (6 of 41) of subjects who had a positive UroAmplitude disease classification but negative cystoscopy. Among predicted high-risk patients, 50% had a clinical recurrence (mean time to recurrence 35.3 mo), all of which were HG. One notable high-risk patient with an initial TaLG tumor experienced a T4aHG recurrence with invasion into the prostate. uGCP-based recurrence prediction anticipated this clinical diagnosis by 17.8 months. Among 35 predicted low-risk patients, only 4 experienced recurrence (all TaLG; mean time to recurrence 20.5 mo). Recurrence-free survival was significantly worse in uGCP-predicted high-risk vs. low-risk patients (HR 4.5, 95% CI 1.01-20.2; Fig. 1). Among 10 subjects with no detectable mutations, no pathologically confirmed recurrence was observed (mean surveillance follow-up 45.3 mo).
Conclusions: uCGP can predict future recurrence of high-risk UC with substantial lead time. If validated with further studies, uCGP may provide a powerful way to risk-stratify patients and enable strategies for intensification (or deintensification) of UC management based on genomic risk.
Source of Funding: Convergent Genomics, Inc.

.jpg)
.jpg)