Back
Poster, Podium & Video Sessions
Moderated Poster
MP54: Bladder Cancer: Non-invasive II
MP54-17: Timing of Radical Cystectomy for BCG Failure
Monday, May 16, 2022
8:45 AM – 10:00 AM
Location: Room 228
Patrick Hensley*, Niyati Lobo, Kelly Bree, Akshay Sood, Neema Navai, Colin Dinney, Ashish Kamat, Houston, TX

Patrick Hensley, MD
University of Texas MD Anderson Cancer Center
Poster Presenter(s)
Introduction: We examine how the timing of radical cystectomy (RC) in a cohort of uniformly treated patients who recur despite intravesical bacillus Calmette-Guérin (BCG) therapy impacts oncologic outcomes.
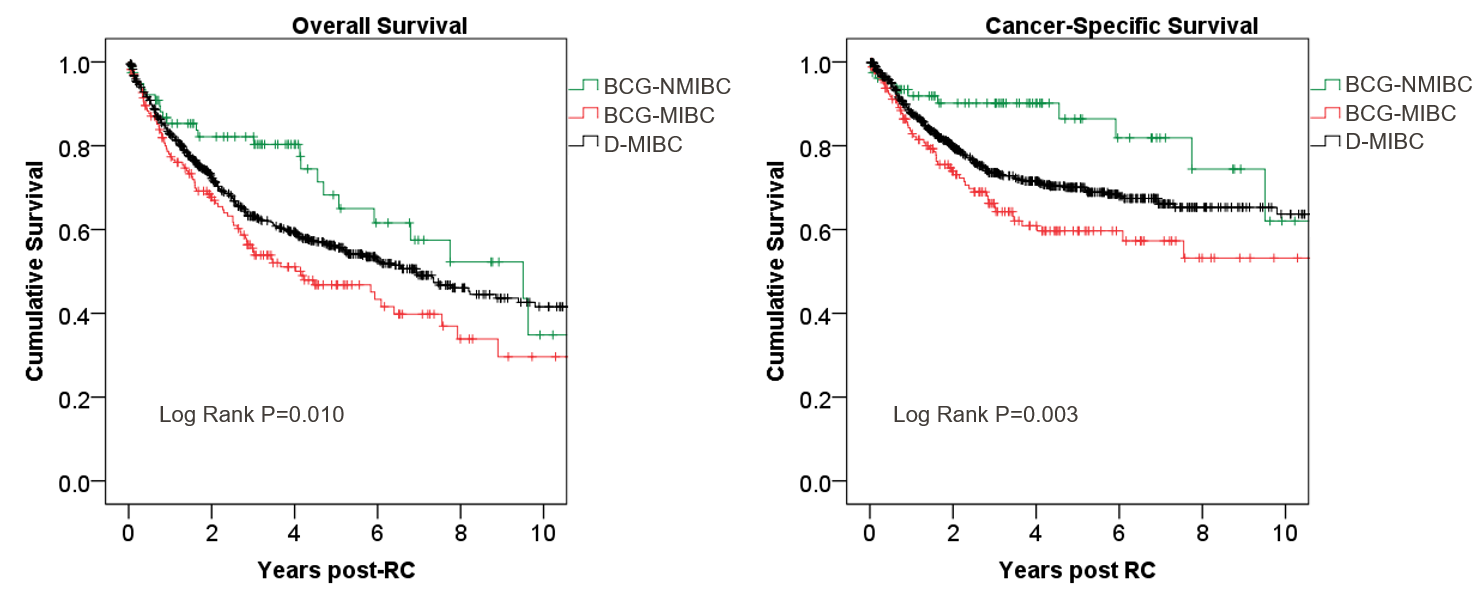
Methods: An institutional review of patients who underwent radical cystectomy (RC) for =cT3N0 urothelial carcinoma of the bladder from 2005-2020 was performed. Patients received at least induction BCG and were categorized as either BCG-nonmuscle-invasive bladder cancer (BCG-NMIBC; =cT1 after BCG) vs. BCG-muscle-invasive bladder cancer (BCG-MIBC; progression to =cT2 disease after BCG) based on clinical stage prior to RC. Patients who underwent RC for de novo MIBC (D-MIBC) were included as a comparator. Kaplan-Meier analysis estimated median overall survival (OS) and cancer-specific survival (CSS). Comparison of time-to-event endpoints was done using the log-rank test.
Results: 78 patients with BCG-NMIBC, 167 with BCG-MIBC, and 637 with D-MIBC were included. Median follow-up after RC was 2.8 years. 446 (55%) MIBC patients received neoadjuvant chemotherapy according to our institutional risk-stratified approach. 69 (88%) NMIBC patients met the FDA definition of ‘BCG unresponsive disease’. Rates of =(y)pT3 disease at RC were 12%; 46%; 39% (p < 0.001) and for (y)N+ disease were 5%; 27%; 20% (p < 0.001) for BCG-NMIBC; BCG-MIBC; D-MIBC, respectively. Median OS was 9.5 years (95% CI 5.3-13.7), 4.1 years (95% CI 2.1-6.2), and 6.9 years (95% CI 5.6-8.3) for BCG-NMIBC; BCG-MIBC; D-MIBC, respectively (Figure). There were no survival differences following RC between patients meeting the following criteria for BCG unresponsive NMIBC: (1) residual/recurrent CIS, (2) recurrent HG Ta/1, or (3) persistent/new HG T1 disease.
Conclusions: Patients who undergo RC for recurrent NMIBC after BCG failure, but prior to progression to MIBC, exhibit favorable pathologic stage and survival outcomes relative to those who progress to MIBC on BCG. Our data emphasize the importance of vigilance, accurate clinical staging and timely intervention in patients who exhibit BCG failure.
Source of Funding: This research was supported by the Wayne B. Duddlesten Professorship in Cancer Research, the Raymond and Maria Floyd Bladder Cancer Research Foundation Grant, NIH/NCI UTMD Anderson SPORE in Genitourinary Cancer (P50CA091846), the Cancer Center Support Grant (NCI Grant P30 CA016672), and a Urology Care Foundation Research Scholars Award (IRG 85-001-25).
Methods: An institutional review of patients who underwent radical cystectomy (RC) for =cT3N0 urothelial carcinoma of the bladder from 2005-2020 was performed. Patients received at least induction BCG and were categorized as either BCG-nonmuscle-invasive bladder cancer (BCG-NMIBC; =cT1 after BCG) vs. BCG-muscle-invasive bladder cancer (BCG-MIBC; progression to =cT2 disease after BCG) based on clinical stage prior to RC. Patients who underwent RC for de novo MIBC (D-MIBC) were included as a comparator. Kaplan-Meier analysis estimated median overall survival (OS) and cancer-specific survival (CSS). Comparison of time-to-event endpoints was done using the log-rank test.
Results: 78 patients with BCG-NMIBC, 167 with BCG-MIBC, and 637 with D-MIBC were included. Median follow-up after RC was 2.8 years. 446 (55%) MIBC patients received neoadjuvant chemotherapy according to our institutional risk-stratified approach. 69 (88%) NMIBC patients met the FDA definition of ‘BCG unresponsive disease’. Rates of =(y)pT3 disease at RC were 12%; 46%; 39% (p < 0.001) and for (y)N+ disease were 5%; 27%; 20% (p < 0.001) for BCG-NMIBC; BCG-MIBC; D-MIBC, respectively. Median OS was 9.5 years (95% CI 5.3-13.7), 4.1 years (95% CI 2.1-6.2), and 6.9 years (95% CI 5.6-8.3) for BCG-NMIBC; BCG-MIBC; D-MIBC, respectively (Figure). There were no survival differences following RC between patients meeting the following criteria for BCG unresponsive NMIBC: (1) residual/recurrent CIS, (2) recurrent HG Ta/1, or (3) persistent/new HG T1 disease.
Conclusions: Patients who undergo RC for recurrent NMIBC after BCG failure, but prior to progression to MIBC, exhibit favorable pathologic stage and survival outcomes relative to those who progress to MIBC on BCG. Our data emphasize the importance of vigilance, accurate clinical staging and timely intervention in patients who exhibit BCG failure.
Source of Funding: This research was supported by the Wayne B. Duddlesten Professorship in Cancer Research, the Raymond and Maria Floyd Bladder Cancer Research Foundation Grant, NIH/NCI UTMD Anderson SPORE in Genitourinary Cancer (P50CA091846), the Cancer Center Support Grant (NCI Grant P30 CA016672), and a Urology Care Foundation Research Scholars Award (IRG 85-001-25).

.jpg)
.jpg)