Back
Poster, Podium & Video Sessions
Moderated Poster
MP56: Bladder Cancer: Invasive V
MP56-04: The role of FDG PET in the staging of bladder cancer patients candidate for radical cystectomy
Monday, May 16, 2022
10:30 AM – 11:45 AM
Location: Room 228
Luigi Nocera*, Giuseppe Basile, Riccardo Leni, Mario De Angelis, Alberto Martini, Simone Scuderi, Giorgio Gandaglia, Milan, Italy, Alex Mottrie, Aalst, Belgium, Andrea Gallina, Lugano, Switzerland, Daniele Raggi, Laura Marandino, Andrea Necchi, Francesco Montorsi, Alberto Briganti, Marco Moschini, Milan, Italy

Luigi Nocera
Vita-Salute San Raffaele University, San Raffaele Hospital
Poster Presenter(s)
Introduction: To date limited evidences are available regarding the potential role of FDG PET in the staging of patients affected by bladder cancer (BCa) who are candidate for radical cystectomy (RC). Indeed, CT scan may not be accurate enough for the detection of lymph node involvement. We hypothesized that FDG PET may be superior to CT scan in the setting of primary staging in BCa.
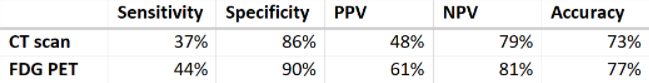
Methods: We identified 231 patients who underwent RC for BCa at our tertiary-care, referral center hospital from January 2015 to September 2021. All patients underwent CT scan and FDG PET for primary staging prior to surgery. All patients were treated by the same highly experienced surgeons. Similarly, the same lymph node dissection template was applied to all patients. Sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV) and accuracy were calculated for both CT scan and FDG PET, relative to histopathological findings at RC.
Results: Of the 231 included patients, 200 (87%) were males, and median age was 68 years (IQR 62-74). 40 patients (17%) were current smokers, while 121 (54%) were former smokers, 110 (48%) received neoadjuvant therapy, and 145 (63%) underwent robotic-assisted RC. At radical cystectomy, 72 (31%), 38 (16%), 14 (6%), 34 (15%), 53 (23%) and 20 (9%) patients harbored respectively pT0, pTa/is, pT1, pT2, pT3 and pT4 disease. 71 patients (31%) also harbored CIS, while 167 (72%) harbored pN0 stage. When comparing CT scan and FDG PET in the setting of primary staging (Table 1), the latter was superior in terms of sensitivity (44 vs 37%), specificity (90 vs 86%), PPV (61 vs 48%), NPV (81 vs 79%) and accuracy (77 vs 73%). However, lymph node involvement was not detected by both imaging tests in a considerable proportion of patients (6%). This observation was particularly evident for lymph nodes in the obturator fossa.
Conclusions: FDG PET represents a very useful tool in the setting of primary staging of bladder cancer patients. However, although FDG PET was superior to traditional imaging (CT scan) in terms of sensitivity, specificity, PPV, NPV and accuracy for the detection of lymph node involvement, the performances of the test were suboptimal. Therefore, other imaging or molecular tools are warranted to improve diagnostic ability in the setting of bladder cancer and thus optimize treatment strategies.
Source of Funding: None.
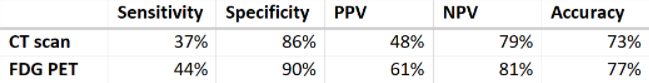
Methods: We identified 231 patients who underwent RC for BCa at our tertiary-care, referral center hospital from January 2015 to September 2021. All patients underwent CT scan and FDG PET for primary staging prior to surgery. All patients were treated by the same highly experienced surgeons. Similarly, the same lymph node dissection template was applied to all patients. Sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV) and accuracy were calculated for both CT scan and FDG PET, relative to histopathological findings at RC.
Results: Of the 231 included patients, 200 (87%) were males, and median age was 68 years (IQR 62-74). 40 patients (17%) were current smokers, while 121 (54%) were former smokers, 110 (48%) received neoadjuvant therapy, and 145 (63%) underwent robotic-assisted RC. At radical cystectomy, 72 (31%), 38 (16%), 14 (6%), 34 (15%), 53 (23%) and 20 (9%) patients harbored respectively pT0, pTa/is, pT1, pT2, pT3 and pT4 disease. 71 patients (31%) also harbored CIS, while 167 (72%) harbored pN0 stage. When comparing CT scan and FDG PET in the setting of primary staging (Table 1), the latter was superior in terms of sensitivity (44 vs 37%), specificity (90 vs 86%), PPV (61 vs 48%), NPV (81 vs 79%) and accuracy (77 vs 73%). However, lymph node involvement was not detected by both imaging tests in a considerable proportion of patients (6%). This observation was particularly evident for lymph nodes in the obturator fossa.
Conclusions: FDG PET represents a very useful tool in the setting of primary staging of bladder cancer patients. However, although FDG PET was superior to traditional imaging (CT scan) in terms of sensitivity, specificity, PPV, NPV and accuracy for the detection of lymph node involvement, the performances of the test were suboptimal. Therefore, other imaging or molecular tools are warranted to improve diagnostic ability in the setting of bladder cancer and thus optimize treatment strategies.
Source of Funding: None.

.jpg)
.jpg)