Back
Poster, Podium & Video Sessions
Moderated Poster
MP56: Bladder Cancer: Invasive V
MP56-06: Associations between Skeletal Muscle Gauge and Survival Following Radical Cystectomy for Bladder Cancer: A Novel Assessment of Muscle Mass and Quality
Monday, May 16, 2022
10:30 AM – 11:45 AM
Location: Room 228
Meghana Noonavath*, Kevin Mun, Seattle, WA, J. Peter Marquardt, Florian J. Fintelmann, Boston, MA, Ryan O'Malley, Sarah K. Holt, Erin Dwyer, Reno Maldonado, Seattle, WA, Leonidas Diamantopoulos, Pittsburgh, PA, Dimitrios Makrakis, Grace Laidlaw, George R. Schade, Dan W. Lin, Jonathan L. Wright, John L. Gore, Yaw Nyame, Petros Grivas, Evan Yu, Bruce Montgomery, Andrew C. Hsieh, Todd A. Yezefski, Michael Schweizer, Heather H. Cheng, Sarah P. Psutka, Seattle, WA

Meghana Noonavath, BS
University of Washington School of Medicine
Poster Presenter(s)
Introduction: Skeletal muscle gauge (SMG) is a novel composite measure that integrates measures of both muscle quantity and quality and is associated with adverse outcomes in patients with nonurologic cancers. SMG is calculated as the product of skeletal muscle index (cross-sectional area of lumbar musculature (cm2/m2)) and mean skeletal muscle density (Hounsfield units). We evaluated associations between presurgical SMG and overall survival (OS) after radical cystectomy (RC) for bladder cancer.
Methods: We retrospectively identified patients with pT1-4 Nx/0 Mx/0 bladder cancer treated with RC with or without neoadjuvant chemotherapy (NAC) with available digitized presurgical imaging (within 75 days of surgery, following NAC if received). Skeletal muscle composition values were obtained from preoperative computed tomography scans performed at the third lumbar vertebrae level per validated methodology. OS from date of surgery was estimated with the Kaplan Meier method and associations with OS were evaluated in univariable and multivariate Cox proportionate hazards models adjusted for age, sex, receipt of NAC, pT stage, Charlson comorbidity index, and performance status.
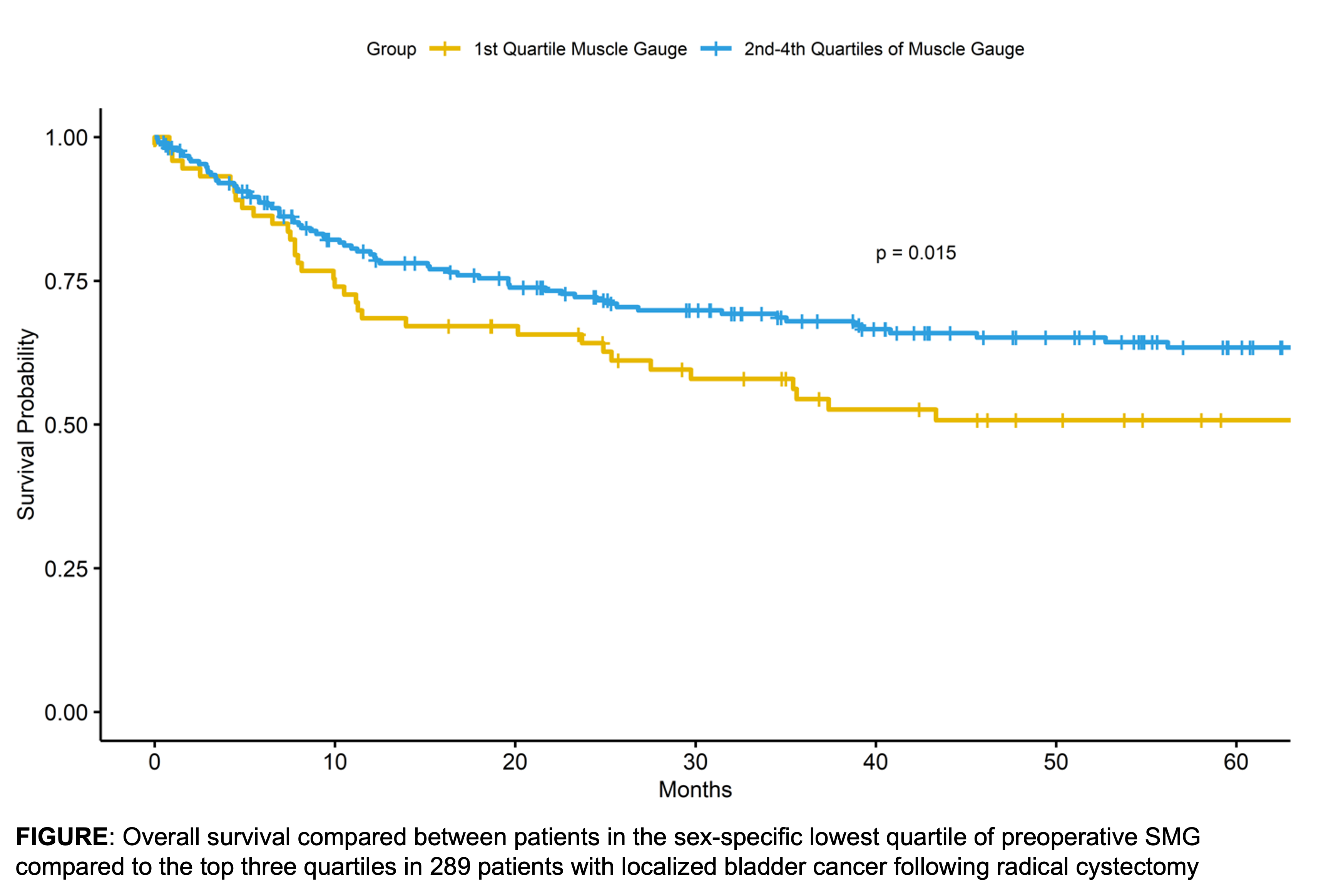
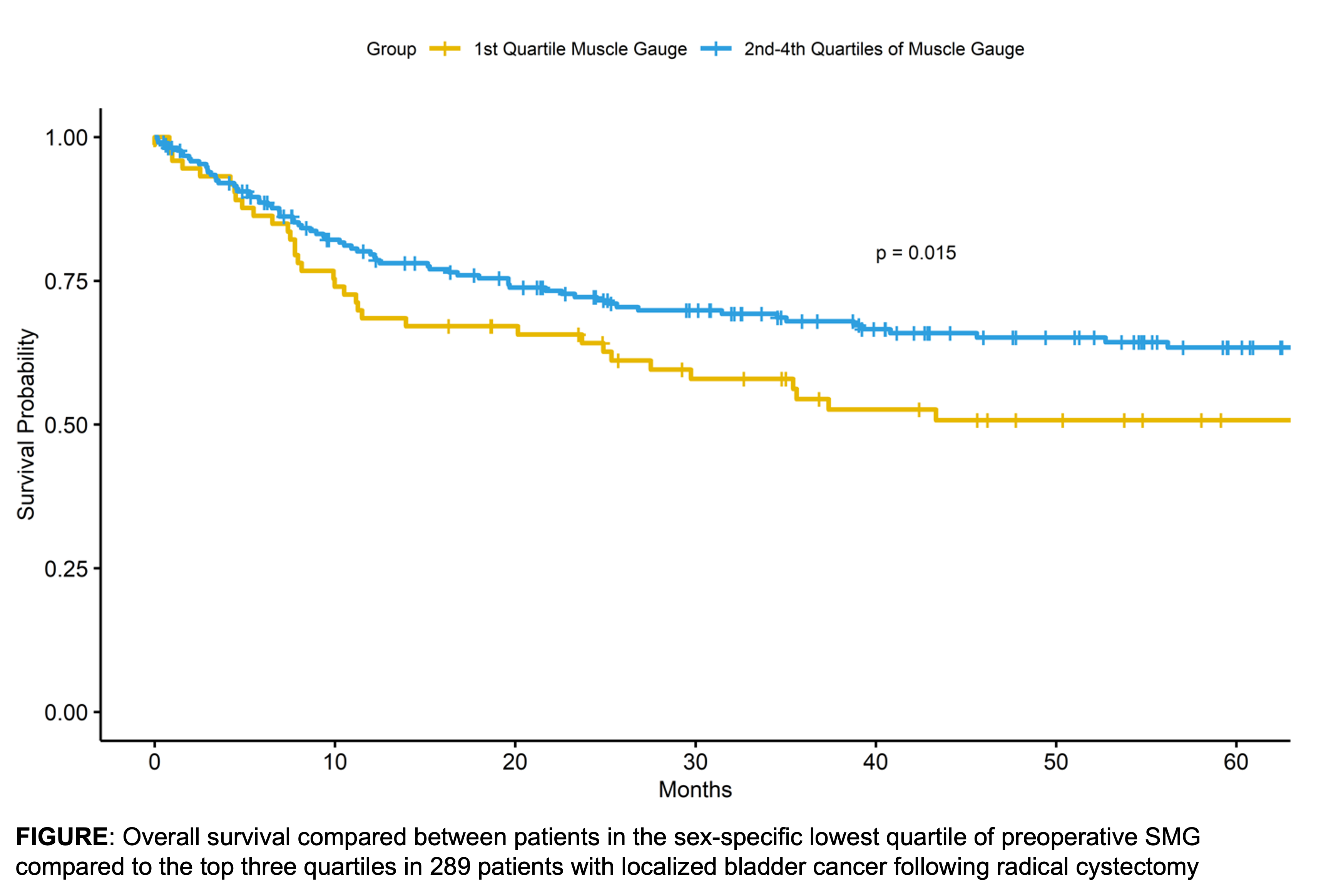
Results: We identified 289 patients (64 women; 61% received NAC) with a median age of 67 years at surgery. Median follow-up was 34 months. Median SMG was 2123.5 (IQR 744.9) in men and 1447.3 (IQR 686) in women. Lower preoperative SMG was associated with older age (p < 0.0001), and receipt of NAC (p=0.03). On univariable analysis, having preoperative SMG in the lowest quartile stratified by sex was associated with decreased OS (HR: 1.55, 95% CI 1.06-2.27, Figure); however, SMG trended toward, but did not retain significance when adjusted for other important covariates (HR: 1.35, 95% CI 0.89-2.04).
Conclusions: Preoperative SMG is a novel composite body composition metric that reflects both skeletal muscle mass and quality. In our study, it was associated with receipt of NAC and older age and demonstrated a trend toward association with decreased OS. Limitations include modest sample size, retrospective nature, possible selection and confounding biases. Future work with larger cohorts will investigate the clinical validity and utility of SMG compared with or added to other measures of muscle mass.
Source of Funding: American Urological Association Summer Medical Student Fellowship
AOA Carolyn L. Kuckein Student Research Fellowship
Methods: We retrospectively identified patients with pT1-4 Nx/0 Mx/0 bladder cancer treated with RC with or without neoadjuvant chemotherapy (NAC) with available digitized presurgical imaging (within 75 days of surgery, following NAC if received). Skeletal muscle composition values were obtained from preoperative computed tomography scans performed at the third lumbar vertebrae level per validated methodology. OS from date of surgery was estimated with the Kaplan Meier method and associations with OS were evaluated in univariable and multivariate Cox proportionate hazards models adjusted for age, sex, receipt of NAC, pT stage, Charlson comorbidity index, and performance status.
Results: We identified 289 patients (64 women; 61% received NAC) with a median age of 67 years at surgery. Median follow-up was 34 months. Median SMG was 2123.5 (IQR 744.9) in men and 1447.3 (IQR 686) in women. Lower preoperative SMG was associated with older age (p < 0.0001), and receipt of NAC (p=0.03). On univariable analysis, having preoperative SMG in the lowest quartile stratified by sex was associated with decreased OS (HR: 1.55, 95% CI 1.06-2.27, Figure); however, SMG trended toward, but did not retain significance when adjusted for other important covariates (HR: 1.35, 95% CI 0.89-2.04).
Conclusions: Preoperative SMG is a novel composite body composition metric that reflects both skeletal muscle mass and quality. In our study, it was associated with receipt of NAC and older age and demonstrated a trend toward association with decreased OS. Limitations include modest sample size, retrospective nature, possible selection and confounding biases. Future work with larger cohorts will investigate the clinical validity and utility of SMG compared with or added to other measures of muscle mass.
Source of Funding: American Urological Association Summer Medical Student Fellowship
AOA Carolyn L. Kuckein Student Research Fellowship

.jpg)
.jpg)