Back
Poster, Podium & Video Sessions
Moderated Poster
MP57: Prostate Cancer: Localized: Surgical Therapy IV
MP57-02: MRI versus Non-MRI Diagnostic Pathways before Radical Prostatectomy: Impact on Nerve-Sparing, Positive Surgical Margins, and Biochemical Recurrence
Monday, May 16, 2022
10:30 AM – 11:45 AM
Location: Room 225
Hiten D. Patel, Goran Rac*, Yudai Okabe, Gaurav Pahouja, Shalin Desai, Steven M. Shea, Alex Gorbonos, Marcus L. Quek, Robert C. Flanigan, Ari Goldberg, Gopal N. Gupta, Maywood, IL

Goran Rac, MD
Loyola University Medical Center
Poster Presenter(s)
Introduction: Multiparametric MRI-TRUS fusion-guided biopsy has improved detection of clinically significant prostate cancer (csPCa). However, the impact of MRI on surgical outcomes is less well established. We compared MRI and non-MRI diagnostic pathways among patients receiving radical prostatectomy (RP) for the performance of bilateral nerve-sparing, positive surgical margin rates, and biochemical recurrence (BCR).
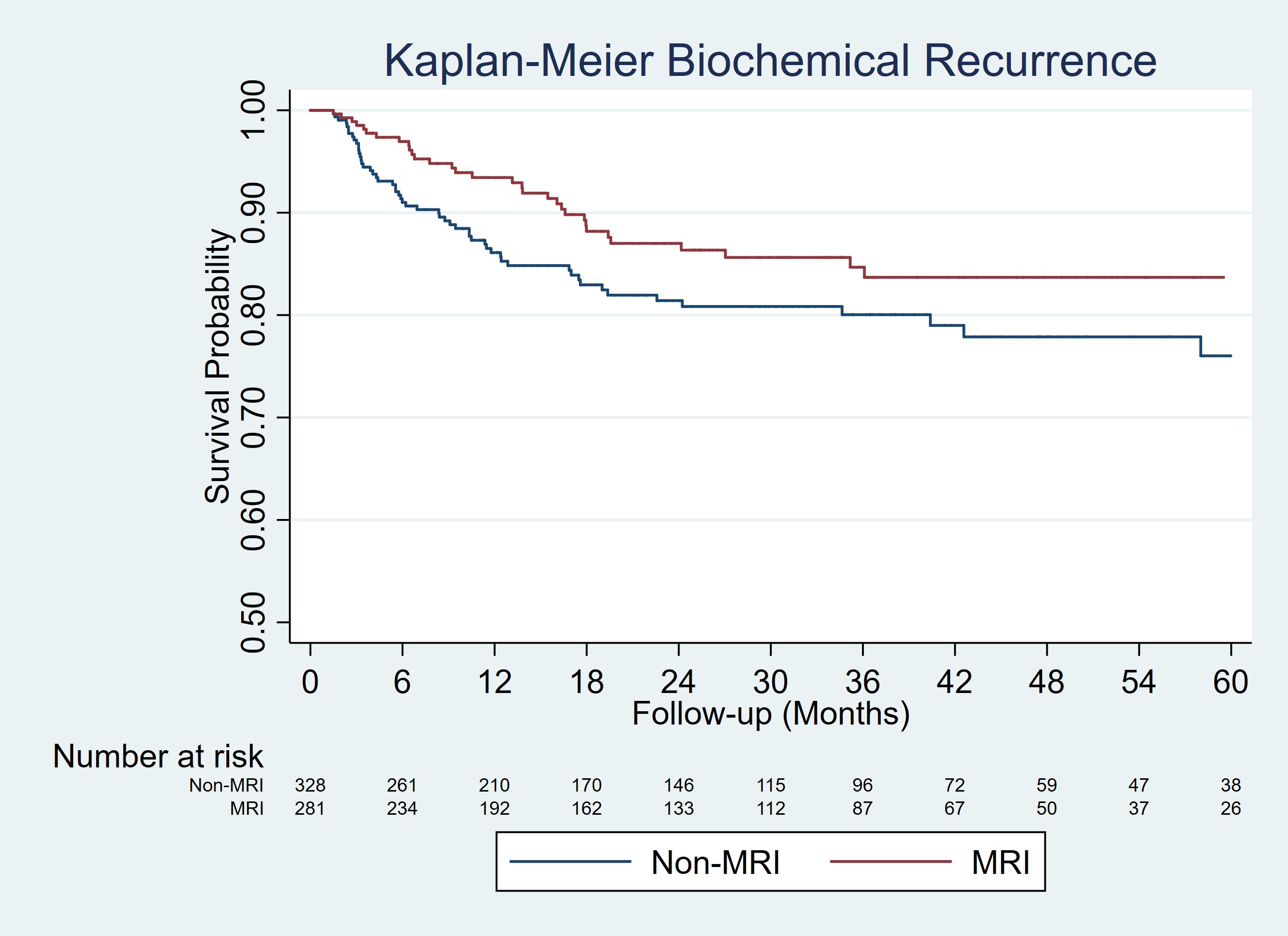
Methods: Men diagnosed with PCa and receiving RP at LUMC (2014-2021) were included. Patients were categorized into MRI or non-MRI diagnostic pathways based on receipt of MRI before prostate biopsy based on clinical suspicion of prostate cancer. Clinical variables included age, race, DRE, PSA, grade group (GG) on biopsy , and surgical and pathologic data. Multivariable logistic regression models evaluated receipt of bilateral nerve-sparing and positive surgical margin rates. Kaplan-Meier curves and Cox proportional hazards regression evaluated BCR.
Results: Of 609 patients, 281 (46.1%) were in the MRI and 328 (53.9%) in the non-MRI groups. MRI patients had lower rates of positive DRE (10.3% vs. 20.7%, p<0.001) but similar PSA (median 6.9 vs. 6.1, p=0.60) and biopsy GG distribution (GG=3: 39.9% vs. 36.0%) compared to non-MRI patients. Pathologic findings were comparable for RP GG (GG=3: 28.5% vs. 28.4%), pT stage (=pT3a: 54.1% vs. 57.3%), and prostate cancer volume (median 15% vs. 15%, p=0.20). Positive surgical margin rates were slightly lower but not significantly different for the MRI and non-MRI groups (22.8% vs. 26.8%, p=0.25) including on multivariable analysis (OR 0.80 (95%CI 0.56-1.17), p=0.25). Bilateral nerve-sparing rates were higher for the MRI vs. non-MRI groups (69.3% vs. 60.1%, p=0.04) including on multivariable analysis (OR 1.95 (95%CI 1.32-2.88), p=0.001). The MRI group demonstrated improved BCR (HR 0.63 (95%CI 0.40-0.99), p=0.04) after adjustment for age, PSA, RP GG, pT stage, and positive surgical margin status.
Conclusions: A multiparametric MRI-based diagnostic approach was associated with similar positive surgical margin rates but greater utilization of bilateral nerve-sparing at RP compared to a non-MRI approach. Cancer control based on BCR favored the MRI group even after adjustment for known prognostic factors.
Source of Funding: Efforts to support data extraction and maintenance of The Prospective Loyola University mpMRI Prostate Biopsy Cohort database is supported by funding from Siemens Medical Solutions USA, Inc.
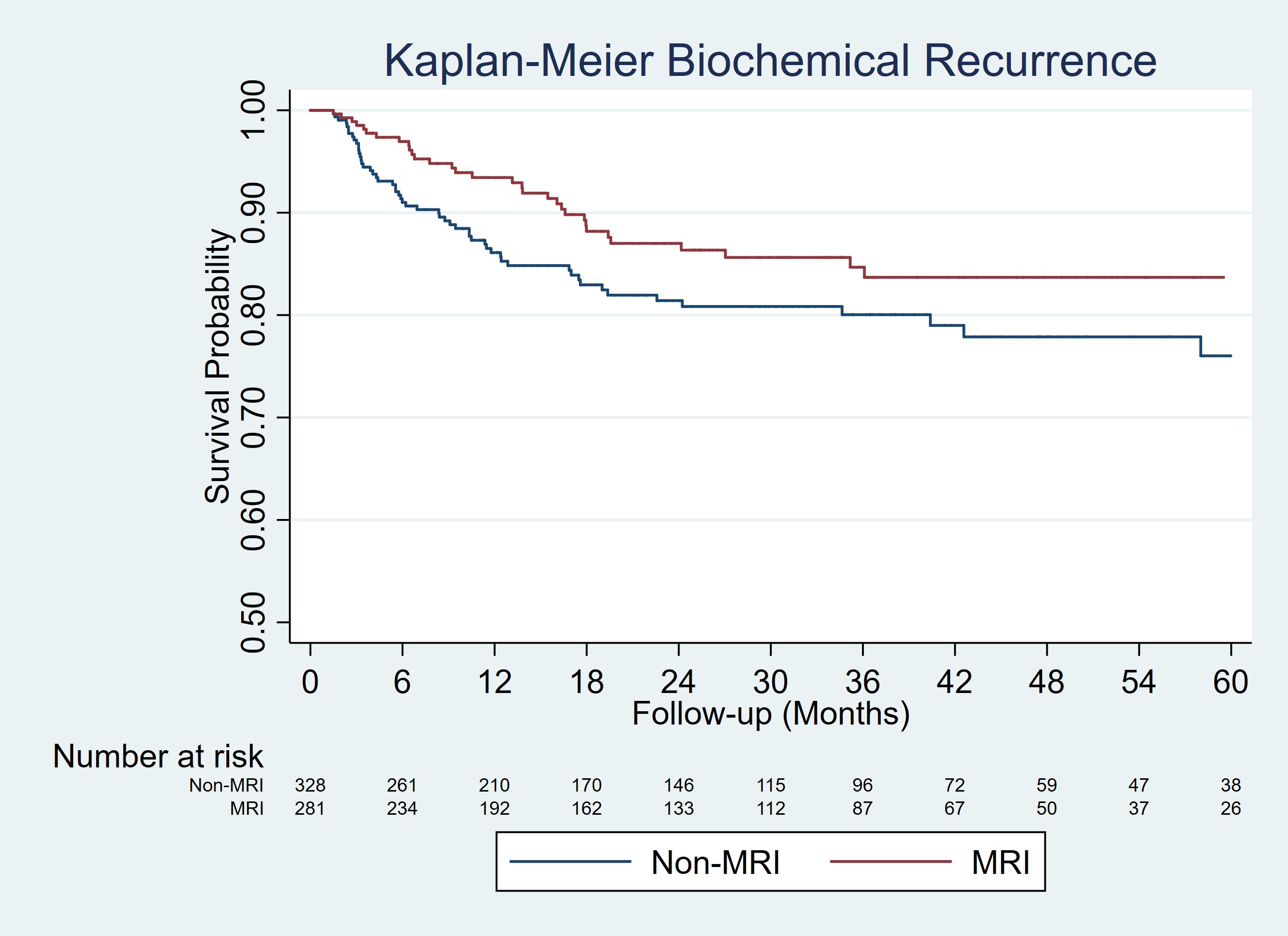
Methods: Men diagnosed with PCa and receiving RP at LUMC (2014-2021) were included. Patients were categorized into MRI or non-MRI diagnostic pathways based on receipt of MRI before prostate biopsy based on clinical suspicion of prostate cancer. Clinical variables included age, race, DRE, PSA, grade group (GG) on biopsy , and surgical and pathologic data. Multivariable logistic regression models evaluated receipt of bilateral nerve-sparing and positive surgical margin rates. Kaplan-Meier curves and Cox proportional hazards regression evaluated BCR.
Results: Of 609 patients, 281 (46.1%) were in the MRI and 328 (53.9%) in the non-MRI groups. MRI patients had lower rates of positive DRE (10.3% vs. 20.7%, p<0.001) but similar PSA (median 6.9 vs. 6.1, p=0.60) and biopsy GG distribution (GG=3: 39.9% vs. 36.0%) compared to non-MRI patients. Pathologic findings were comparable for RP GG (GG=3: 28.5% vs. 28.4%), pT stage (=pT3a: 54.1% vs. 57.3%), and prostate cancer volume (median 15% vs. 15%, p=0.20). Positive surgical margin rates were slightly lower but not significantly different for the MRI and non-MRI groups (22.8% vs. 26.8%, p=0.25) including on multivariable analysis (OR 0.80 (95%CI 0.56-1.17), p=0.25). Bilateral nerve-sparing rates were higher for the MRI vs. non-MRI groups (69.3% vs. 60.1%, p=0.04) including on multivariable analysis (OR 1.95 (95%CI 1.32-2.88), p=0.001). The MRI group demonstrated improved BCR (HR 0.63 (95%CI 0.40-0.99), p=0.04) after adjustment for age, PSA, RP GG, pT stage, and positive surgical margin status.
Conclusions: A multiparametric MRI-based diagnostic approach was associated with similar positive surgical margin rates but greater utilization of bilateral nerve-sparing at RP compared to a non-MRI approach. Cancer control based on BCR favored the MRI group even after adjustment for known prognostic factors.
Source of Funding: Efforts to support data extraction and maintenance of The Prospective Loyola University mpMRI Prostate Biopsy Cohort database is supported by funding from Siemens Medical Solutions USA, Inc.

.jpg)
.jpg)