Back
Poster, Podium & Video Sessions
Moderated Poster
MP58: Prostate Cancer: Detection & Screening VII
MP58-02: PSA-Density Determines the Need for Systematic Biopsy in Men with PI-RADS 4/5 MRI
Monday, May 16, 2022
1:00 PM – 2:15 PM
Location: Room 228
Zachary Feuer*, Richard Huang, Fang-Ming Deng, James Wysock, William Huang, Samir Taneja, New York, NY
- ZF
Zachary Feuer, MD, BS
NYU Langone Health
Poster Presenter(s)
Introduction: MRI-targeted biopsy (MRI-TB) improves cancer detection rate (CDR) of clinically significant prostate cancer (csPCa), while reducing detection of Gleason Grade Group (GGG) 1 in men with PI-RADS =3 pre-biopsy MRI. Prior to the adoption of MRI, PSA density (PSAD) was used to risk stratify men. We aim to demonstrate that PSAD stratification helps to identify which men may require systematic biopsy (SB) to improve csPCa CDR.
Methods: All biopsy-naïve men, with PI-RADS =3 MRI undergoing concurrent SB and MRI-TB between 2/2015-9/2019 were included. Men were excluded if they had non-concurrent SB/MRI-TB or no reported MRI-based prostate volume. csPCa was defined as =GGG2. PI-RADS 4/5 were grouped. CDR were calculated for combined, and unique SB and MRI-TB csPCa, while additive value was determined by subtracting unique SB or MRI-TB CDR from combined CDR. 95% confidence intervals (CI) for CDR were calculated using the Clopper-Pearson exact method.
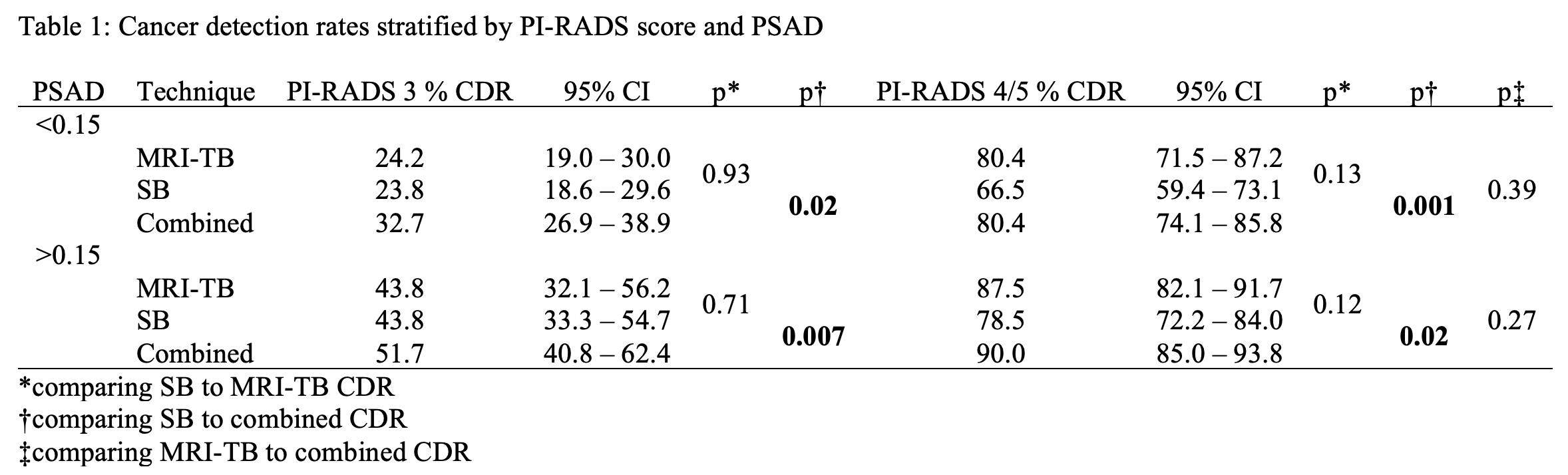
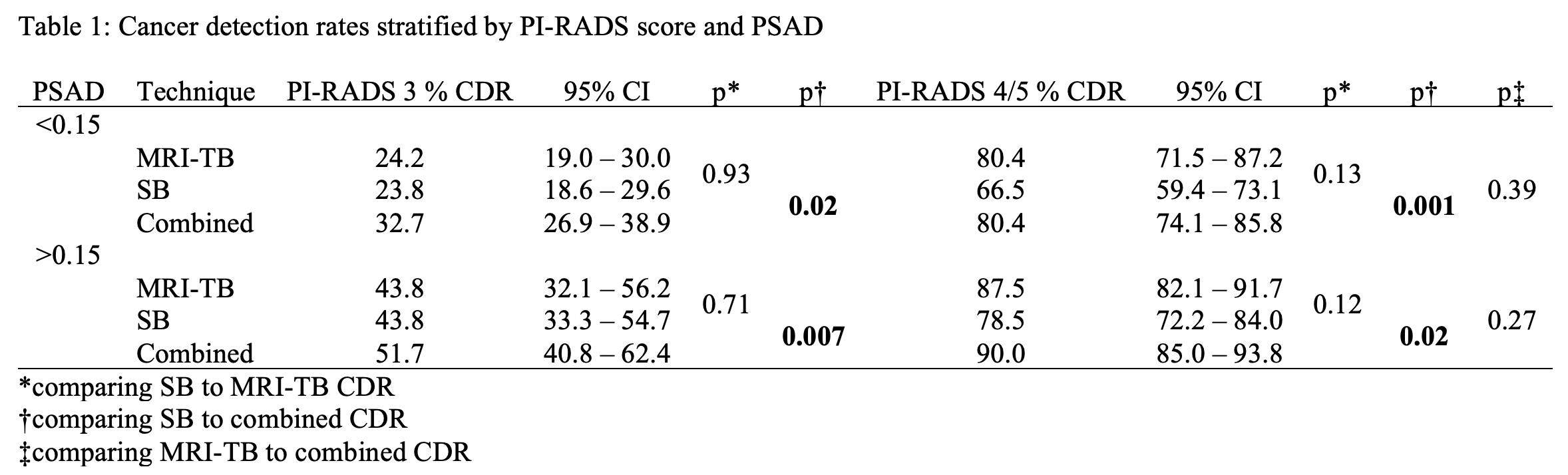
Results: 966 men were included. Median age was 68 years (IQR 66-72), PSA was 6.3 (IQR 4.5-7.4) and PSAD was 0.12 (IQR 0.07-0.18). Results are summarized (Table 1). Amongst men with PI-RADS 3 MRI, CDR were similar for MRI-TB and SB when stratified by PSAD, while combined CDR was improved independent of PSAD strata.
For men with PI-RADS 4/5 and PSAD <0.15, CDR for MRI-TB and SB were 80.4% and 66.5%, respectively (p=0.32). Combined CDR was 80.4%, which was improved from SB alone (p=0.001), but not from MRI-TB alone (p=0.39). 13.9% csPCas was uniquely diagnosed on MRI-TB, while no csPCas were uniquely diagnosed on SB.
For men with PI-RADS 4/5 and PSAD >0.15, CDR for MRI-TB and SB were 87.5% and 78.5%, respectively (p=0.12). Combined CDR was 90.0%, which was improved from SB alone (p=0.02), but not from MRI-TB alone (p=0.27). 11.5% csPCas were uniquely diagnosed on MRI-TB, while 6.2% csPCas were uniquely diagnosed on SB.
Conclusions: Concurrent MRI-TB and SB improves combined csPCa CDR in men with PI-RADS 3 MRI, while CDR for SB/MRI-TB are similar. Amongst men with PI-RADS 4/5 MRI with PSAD <0.15, no unique csPCa was diagnosed on SB, suggesting that SB may be omitted. For those with PSAD >0.15, MRI-TB and SB contributed unique csPCa diagnoses to combined CDR, suggesting utility of concurrent use. SB may reduce targeting error in small volume prostates, while the value of random sampling is mitigated as size increases.
Source of Funding: Joseph and Diane Steinberg Charitable Trust
Methods: All biopsy-naïve men, with PI-RADS =3 MRI undergoing concurrent SB and MRI-TB between 2/2015-9/2019 were included. Men were excluded if they had non-concurrent SB/MRI-TB or no reported MRI-based prostate volume. csPCa was defined as =GGG2. PI-RADS 4/5 were grouped. CDR were calculated for combined, and unique SB and MRI-TB csPCa, while additive value was determined by subtracting unique SB or MRI-TB CDR from combined CDR. 95% confidence intervals (CI) for CDR were calculated using the Clopper-Pearson exact method.
Results: 966 men were included. Median age was 68 years (IQR 66-72), PSA was 6.3 (IQR 4.5-7.4) and PSAD was 0.12 (IQR 0.07-0.18). Results are summarized (Table 1). Amongst men with PI-RADS 3 MRI, CDR were similar for MRI-TB and SB when stratified by PSAD, while combined CDR was improved independent of PSAD strata.
For men with PI-RADS 4/5 and PSAD <0.15, CDR for MRI-TB and SB were 80.4% and 66.5%, respectively (p=0.32). Combined CDR was 80.4%, which was improved from SB alone (p=0.001), but not from MRI-TB alone (p=0.39). 13.9% csPCas was uniquely diagnosed on MRI-TB, while no csPCas were uniquely diagnosed on SB.
For men with PI-RADS 4/5 and PSAD >0.15, CDR for MRI-TB and SB were 87.5% and 78.5%, respectively (p=0.12). Combined CDR was 90.0%, which was improved from SB alone (p=0.02), but not from MRI-TB alone (p=0.27). 11.5% csPCas were uniquely diagnosed on MRI-TB, while 6.2% csPCas were uniquely diagnosed on SB.
Conclusions: Concurrent MRI-TB and SB improves combined csPCa CDR in men with PI-RADS 3 MRI, while CDR for SB/MRI-TB are similar. Amongst men with PI-RADS 4/5 MRI with PSAD <0.15, no unique csPCa was diagnosed on SB, suggesting that SB may be omitted. For those with PSAD >0.15, MRI-TB and SB contributed unique csPCa diagnoses to combined CDR, suggesting utility of concurrent use. SB may reduce targeting error in small volume prostates, while the value of random sampling is mitigated as size increases.
Source of Funding: Joseph and Diane Steinberg Charitable Trust

.jpg)
.jpg)