Back
Poster, Podium & Video Sessions
Moderated Poster
MP58: Prostate Cancer: Detection & Screening VII
MP58-11: Comparison of Prostate Cancer Detection Rates Between Trans-rectal MRI/US Fusion and Trans-Perineal Cognitive Targeted Prostate Biopsy Approaches
Monday, May 16, 2022
1:00 PM – 2:15 PM
Location: Room 228
Johnathan Drevik*, Zafardjan Dalimov, Allen Rojhani, Phillip Abbosh, Steven Sterious, Joshua Cohn, Jay Simhan, Justin Friedlander, Eric Ghiraldi, Robert Uzzo, Serge Ginzburg, Philadelphia, PA
Johnathan A. Drevik, MD
Einstein Healthcare Network
Poster Presenter(s)
Introduction: Many urology practices have access to MRI/US fusion technology for prostate targeting via transrectal (TR) approach. The adoption of transperineal (TP) prostate biopsy is increasing, but conversion to TP fusion technology can be financially prohibitive. Cognitive TP targeting is a cost-effective alternative but may be perceived as a barrier and assumed to result in lower cancer detection. We describe a single surgeon’s transition from TR MRI/US fusion to cognitive TP targeted biopsies
Methods: A retrospective chat review of patients that underwent targeted prostate biopsy (either TP cognitive or TR MRI/US fusion) from 2015 - 2021 was performed. Patients with PSA > 20, concomitant procedures or metastatic disease were excluded. In patients with multiple biopsies only the first targeted biopsy was abstracted. Chi-Square and Mann-Whitney tests were utilized for univariable analysis of categorical and continuous variables, respectively. Multivariable logistic regression models were fit to evaluate variables associated with clinically significant prostate cancer on targeted biopsy.
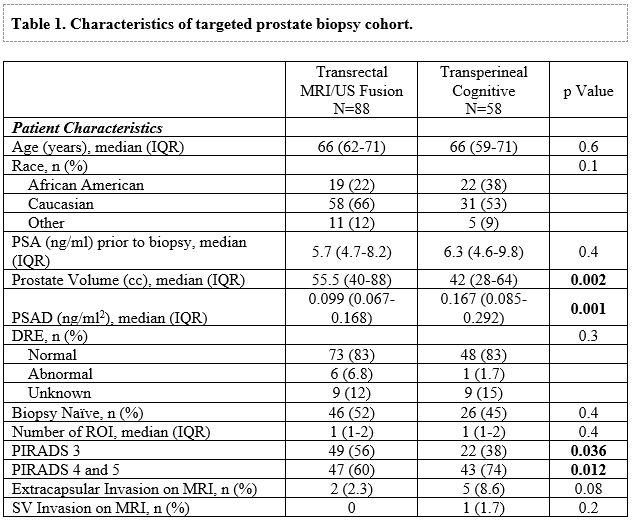
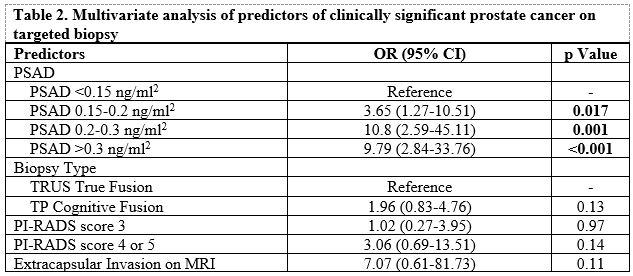
Results: Of the 146 patients that underwent targeted prostate biopsy, 40% underwent TP cognitive approach. Clinicopathologic characteristics between the two groups differed in demographic distribution, prostate size, and MRI findings (Table 1). The detection of any prostate cancer (64% vs 39%, p=0.003) and clinically significant prostate cancer (csPCa) (48% vs 19%, p<0.001) were higher in the TP cognitive targeted group. On multivariable analysis, controlling for clinicopathologic characteristics, only PSA density above >0.15 ng/ml2 was associated with csPCa on targeted biopsy (Table 2). Targeted biopsy approach, TR fusion vs. TP cognitive targeted biopsy, was not associated with detection of csPCa.
Conclusions: Clinically significant prostate cancer detection rate was not compromised when switching from transrectal MRI/US fusion to transperineal cognitive targeted biopsy technique.
Source of Funding: None
Methods: A retrospective chat review of patients that underwent targeted prostate biopsy (either TP cognitive or TR MRI/US fusion) from 2015 - 2021 was performed. Patients with PSA > 20, concomitant procedures or metastatic disease were excluded. In patients with multiple biopsies only the first targeted biopsy was abstracted. Chi-Square and Mann-Whitney tests were utilized for univariable analysis of categorical and continuous variables, respectively. Multivariable logistic regression models were fit to evaluate variables associated with clinically significant prostate cancer on targeted biopsy.
Results: Of the 146 patients that underwent targeted prostate biopsy, 40% underwent TP cognitive approach. Clinicopathologic characteristics between the two groups differed in demographic distribution, prostate size, and MRI findings (Table 1). The detection of any prostate cancer (64% vs 39%, p=0.003) and clinically significant prostate cancer (csPCa) (48% vs 19%, p<0.001) were higher in the TP cognitive targeted group. On multivariable analysis, controlling for clinicopathologic characteristics, only PSA density above >0.15 ng/ml2 was associated with csPCa on targeted biopsy (Table 2). Targeted biopsy approach, TR fusion vs. TP cognitive targeted biopsy, was not associated with detection of csPCa.
Conclusions: Clinically significant prostate cancer detection rate was not compromised when switching from transrectal MRI/US fusion to transperineal cognitive targeted biopsy technique.
Source of Funding: None

.jpg)
.jpg)