Back
Poster, Podium & Video Sessions
Moderated Poster
MP59: Bladder Cancer: Non-Invasive III
MP59-11: En bloc Resection for Bladder Tumors: An Updated Systematic Review and Meta-analyses of its differential effect on its safety, histopathology and, recurrence
Monday, May 16, 2022
1:00 PM – 2:15 PM
Location: Room 225
Takafumi Yanagisawa*, Vienna, Austria, Keiichiro Mori, Tokyo, Japan, Reza Sari Motlagh, Tatsushi Kawada, Hadi Mostafaei, Fahad Quhal, Ekaterina Laukhtina, Pawel Rajwa, Frederik König, Maximilian Pallauf, Benjamin Pradere, David D'Andrea, Eva Compérat, Vienna, Austria, Jun Miki, Takahiro Kimura, Shin Egawa, Tokyo, Japan, Shahrokh F. Shariat, Vienna, Austria
Takafumi Yanagisawa, MD,PhD
Medical University of Vienna
Poster Presenter(s)
Introduction: En bloc resection for bladder tumors (ERBT) has been developed to overcome the shortcomings of conventional transurethral resection of bladder tumors (cTURBT) with regards to safety, pathologic evaluation and oncologic outcomes. However, the potential benefits of utility compared with cTURBT have not been conclusively demonstrated. This systematic review and meta-analysis aimed to update the current evidence with focus on the pathologic benefits of ERBT for non-muscle invasive bladder cancer (NMIBC).
Methods: Multiple databases were searched for articles published before August 2021. Studies were deemed eligible if they compared safety, pathologic and clinical outcomes in patients who underwent ERBT with those who underwent cTURBT.
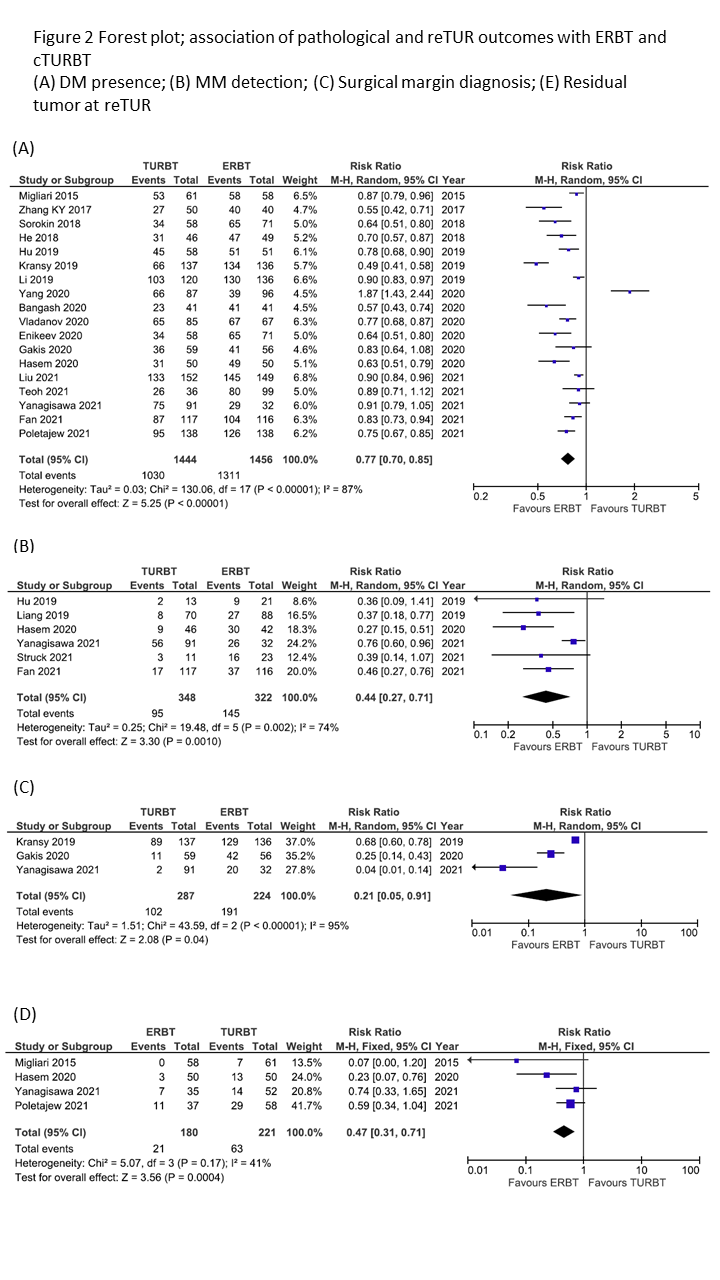
Results: Overall, 13 randomized clinical trials (RCTs) and 16 non-RCTs (NRCTs)/ observational studies comprising 4,484 patients were eligible for this meta-analysis. Among 13 RCTs, the pooled 12- and 24-months recurrence risk ratio (RR) were not different between the two surgical techniques (0.96 [95% Confidence Intervals (CI); 0.74- 1.23] and 0.83 [95% CI; 0.55- 1.23], respectively). The pooled RR for bladder perforation was 0.13 (95% CI; 0.05-0.34) in favor of ERBT. The differential rates of detrusor muscle (DM) presence (Pooled RR: 0.77, 95% CI: 0.70-0.85), of detectable muscularis mucosae (MM) (Pooled RR: 0.44, 95% CI: 0.27-0.71) and of evaluable surgical margins (Pooled RR: 0.28, 95% CI: 0.21-0.38) were all more likely in patients receiving ERBT. Patients who underwent ERBT had a lower rate of residual tumor at repeat TURBT (reTUR) than those treated with cTURBT (RR: 0.47, 95% CI: 0.31- 0.71).
Conclusions: ERBT seems to be safer and to yield superior histopathologic information and performance compared to cTURBT in patients with NMIBC. Despite the failure to improve the recurrence rate, the more accurate histopathologic analysis is likely to improve clinical decision-making and core delivery in NMIBC.
Source of Funding: None.

Methods: Multiple databases were searched for articles published before August 2021. Studies were deemed eligible if they compared safety, pathologic and clinical outcomes in patients who underwent ERBT with those who underwent cTURBT.
Results: Overall, 13 randomized clinical trials (RCTs) and 16 non-RCTs (NRCTs)/ observational studies comprising 4,484 patients were eligible for this meta-analysis. Among 13 RCTs, the pooled 12- and 24-months recurrence risk ratio (RR) were not different between the two surgical techniques (0.96 [95% Confidence Intervals (CI); 0.74- 1.23] and 0.83 [95% CI; 0.55- 1.23], respectively). The pooled RR for bladder perforation was 0.13 (95% CI; 0.05-0.34) in favor of ERBT. The differential rates of detrusor muscle (DM) presence (Pooled RR: 0.77, 95% CI: 0.70-0.85), of detectable muscularis mucosae (MM) (Pooled RR: 0.44, 95% CI: 0.27-0.71) and of evaluable surgical margins (Pooled RR: 0.28, 95% CI: 0.21-0.38) were all more likely in patients receiving ERBT. Patients who underwent ERBT had a lower rate of residual tumor at repeat TURBT (reTUR) than those treated with cTURBT (RR: 0.47, 95% CI: 0.31- 0.71).
Conclusions: ERBT seems to be safer and to yield superior histopathologic information and performance compared to cTURBT in patients with NMIBC. Despite the failure to improve the recurrence rate, the more accurate histopathologic analysis is likely to improve clinical decision-making and core delivery in NMIBC.
Source of Funding: None.

.jpg)
.jpg)