Back
Poster, Podium & Video Sessions
Moderated Poster
MP59: Bladder Cancer: Non-Invasive III
MP59-17: Development and internal validation of a predictive model for recurrence-free survival in pTa low-grade bladder cancer
Monday, May 16, 2022
1:00 PM – 2:15 PM
Location: Room 225
Jorge Daza*, Buffalo, NY, Ralph Grauer, Sophie Chen, Etienne Lavallèe, Shirin Razdan, New York, NY, Linda Dey, Gunnar Steineck, Stockholm, Sweden, Qiang Li, Aly Ahmed, Buffalo, NY, Reza Mehrazin, Nikhil Waingankar, New York, NY, Khurshid Guru, Buffalo, NY, Peter Wiklund, John Sfakianos, New York, NY
- JD
Jorge A. Daza, M.D
Associate Researcher
Roswell Park Comprehensive Cancer Center
Poster Presenter(s)
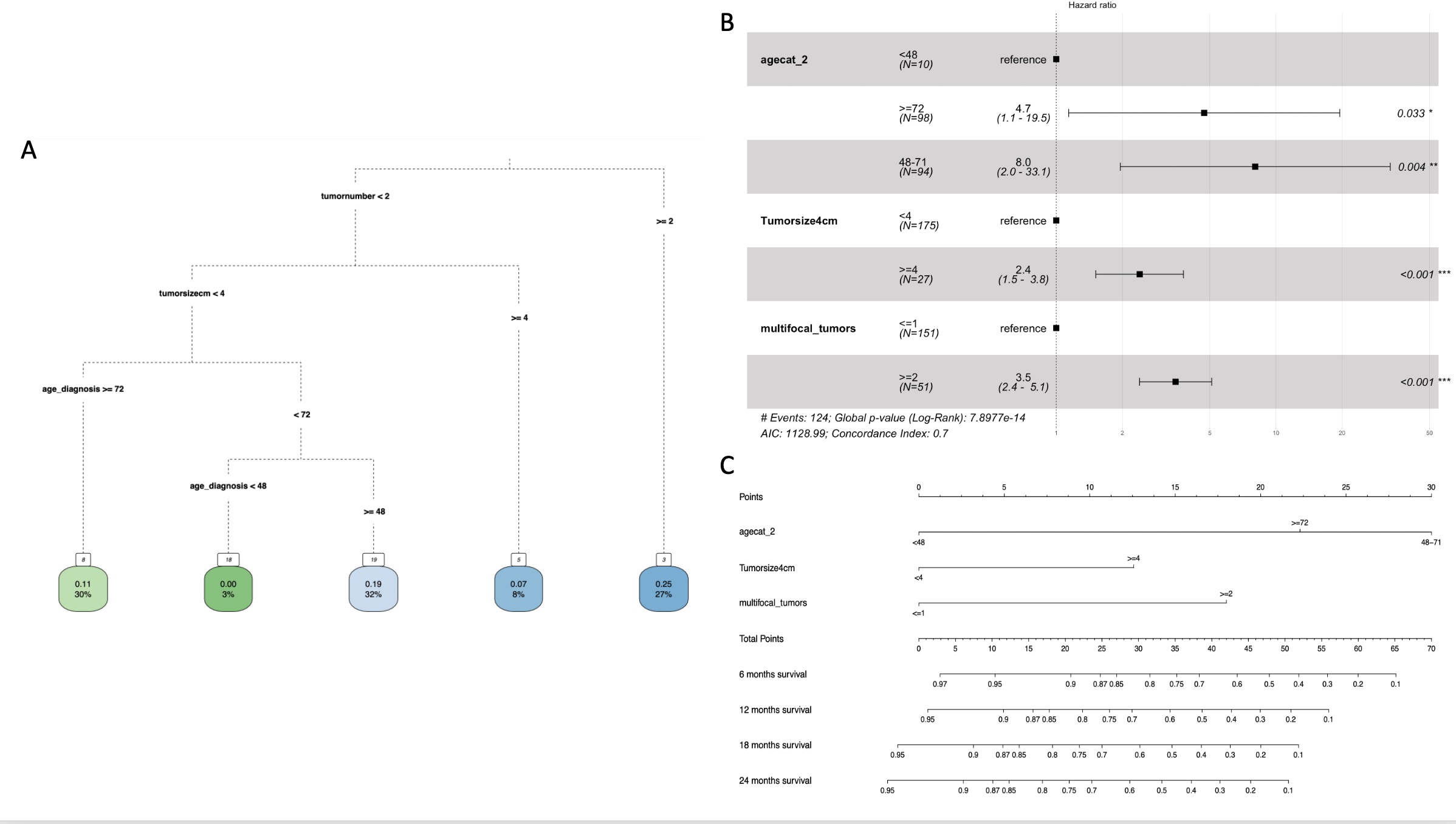
Introduction: Ta low-grade (LG) non-muscle invasive bladder cancer (NMIBC) is a relatively indolent disease for which patients may be subjected to oversurveillance via follow-up cystoscopies. To develop a predictive model associated with recurrence-free survival (RFS) at 6, 12, 18 and 24 months in TaLG cases that consider patients’ risk aversion.
Methods: Analysis was performed on 202 patients with newly diagnosed TaLG NMIBC, who did not receive adjuvant intravesical therapy, from a population-based prospectively maintained database of patients treated in Stockholm County, Sweden. To identify risk groups associated with recurrence, we performed a classification tree analysis using recursive partitioning. To reduce the risk of overfitting the data, we tuned the tree parameters to obtain the lowest cross-validated error. Association between risk groups and RFS was evaluated by Kaplan Meier analysis. A Cox proportional hazard model selected significant risk factors associated with RFS from the risk groups. The model was internally validated and calibrated using 1000 bootstrapped samples. A nomogram to estimate RFS at 6, 12, 18, and 24 months was generated. The performance of our model was compared to EUA/AUA stratification using a decision curve analysis (DCA).
Results: The classification tree found that tumor number, tumor size and age were the most relevant variables associated with recurrence and were significantly associated with RFS in the Cox proportional hazard model. The patients with the highest likelihood of recurrence were those with multifocal (93%) or single = 4cm tumors (92%). DCA analysis showed that our model outperformed EUA/AUA stratification and the treat all/none approaches. We built a nomogram to manually obtain the predicted values from the Cox proportional hazard model. Our model showed appropriate calibration at 6, 12, 18 and 24 months.
Conclusions: We developed a predictive model to identify TaLG patients that benefit from less frequent follow-up cystoscopy schedule based on the estimated RFS and personal recurrence risk aversion. The new model outperformed the AUA/EUA stratification via DCA in terms of net benefit and net reduction in interventions per 100 patients.
Source of Funding: NA
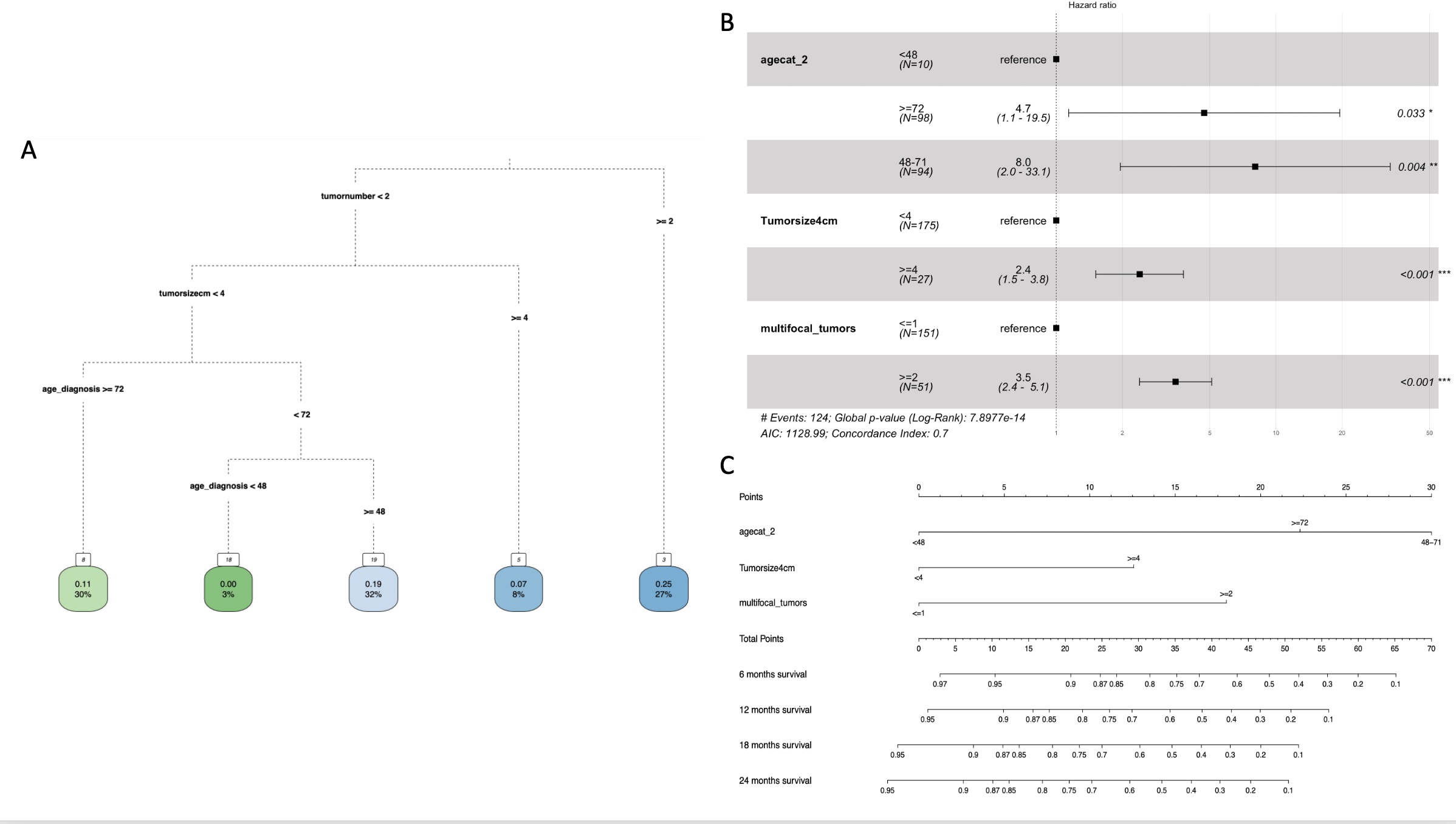
Methods: Analysis was performed on 202 patients with newly diagnosed TaLG NMIBC, who did not receive adjuvant intravesical therapy, from a population-based prospectively maintained database of patients treated in Stockholm County, Sweden. To identify risk groups associated with recurrence, we performed a classification tree analysis using recursive partitioning. To reduce the risk of overfitting the data, we tuned the tree parameters to obtain the lowest cross-validated error. Association between risk groups and RFS was evaluated by Kaplan Meier analysis. A Cox proportional hazard model selected significant risk factors associated with RFS from the risk groups. The model was internally validated and calibrated using 1000 bootstrapped samples. A nomogram to estimate RFS at 6, 12, 18, and 24 months was generated. The performance of our model was compared to EUA/AUA stratification using a decision curve analysis (DCA).
Results: The classification tree found that tumor number, tumor size and age were the most relevant variables associated with recurrence and were significantly associated with RFS in the Cox proportional hazard model. The patients with the highest likelihood of recurrence were those with multifocal (93%) or single = 4cm tumors (92%). DCA analysis showed that our model outperformed EUA/AUA stratification and the treat all/none approaches. We built a nomogram to manually obtain the predicted values from the Cox proportional hazard model. Our model showed appropriate calibration at 6, 12, 18 and 24 months.
Conclusions: We developed a predictive model to identify TaLG patients that benefit from less frequent follow-up cystoscopy schedule based on the estimated RFS and personal recurrence risk aversion. The new model outperformed the AUA/EUA stratification via DCA in terms of net benefit and net reduction in interventions per 100 patients.
Source of Funding: NA

.jpg)
.jpg)