Back
Poster, Podium & Video Sessions
Podium
PD03: Prostate Cancer: Epidemiology & Natural History I
PD03-07: Association Between Adverse Surgical Pathology and Overall Survival Among Patients with Low-Risk Prostate Cancer
Friday, May 13, 2022
8:00 AM – 8:10 AM
Location: Room 245
Grace Lee, Eileen Lee*, Zev Leopold, Sinae Kim, New Brunswick, NJ, Michael S. Leapman, Isaac Y. Kim, New Haven, CT
- EL
Podium Presenter(s)
Introduction: The possibility of adverse surgical pathology among patients with low-risk prostate cancer is often used as a surrogate to determine the suitability of active surveillance (AS) versus definitive local treatment. We aimed to understand the association between adverse pathology and overall survival (OS) among ostensible candidates for AS who were treated with radical prostatectomy.
Methods: We queried the National Cancer Database to identify patients diagnosed with low-risk prostate cancer (Gleason score (GS) 6, clinical stage T1-T2a, and Prostate-Specific Antigen (PSA) <10 ng/mL), who underwent radical prostatectomy from 2004 to 2016. The primary objective was to compare OS between patients with adverse pathology, defined as pathological GS 7+ or pathological stage =T3 and/or N1, compared to those who did not. We used a Kaplan-Meier product limit estimate to determine five and ten-year OS and a log-rank test to compare OS. Adjusted Cox proportional hazard models were used to analyze the association between adverse pathology and survival. Additionally, we used multivariate logistic regression to evaluate pre-operative predictors of adverse pathology.
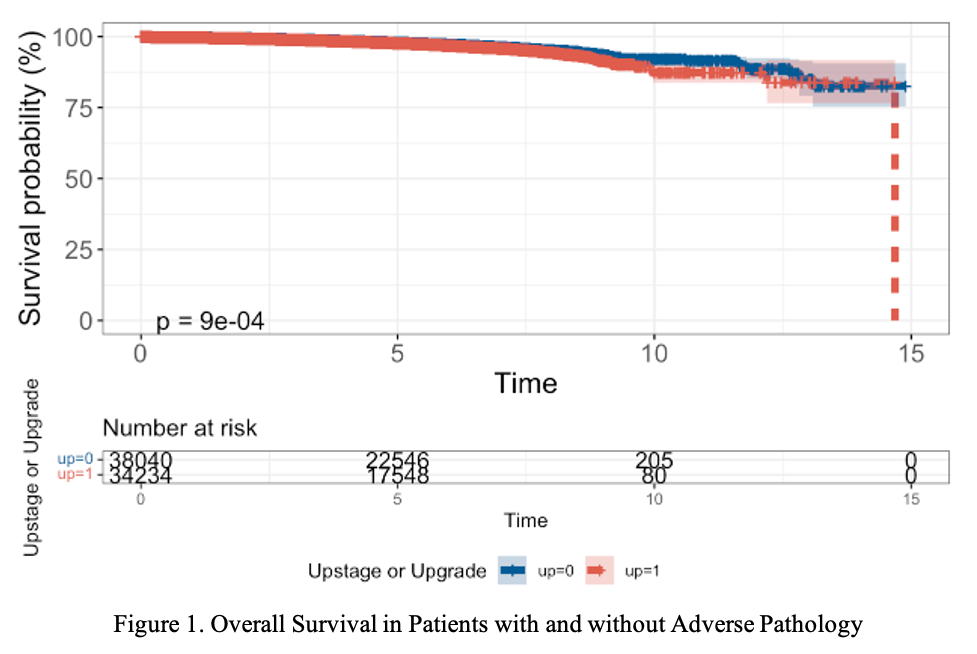
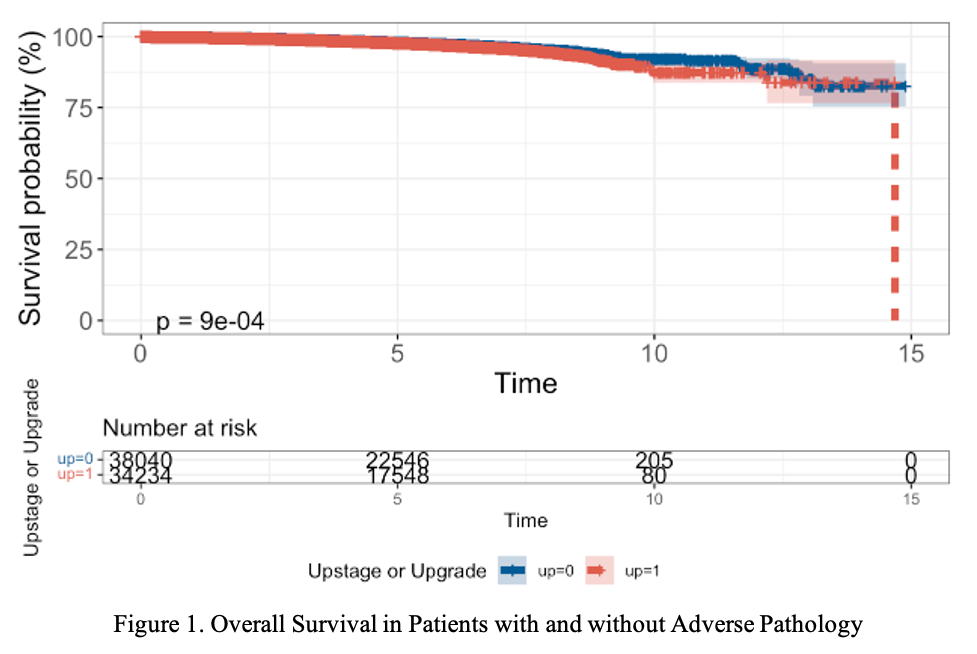
Results: Among low-risk patients treated with prostatectomy (N=72,274), 34,234 (47.4%) experienced pathologic upstage or upgrade. The majority, 83.2%, had pathological GS 7+ disease alone, while 16.7% had both pathological GS 7+ and pT3+/N1, and <0.1% had pT3+ or pN1+ alone. Lower age, White race, higher comorbidity score, lack of insurance, no high school diploma, treatment outside of a community cancer program, Midwest or South relative to Northeast region, and higher PSA were associated with adverse pathology (p <0.001). Five-year OS was 98.0% and 97.8%, while ten-year OS was 92.2% and 87.3% for patients with and without adverse pathology, respectively (Figure 1). On multivariate analysis, neither upstaging nor upgrading was significantly associated with worse OS compared to patients with organ-confined pathology (HR = 1.05, 95% CI = [0.95, 1.15], p = 0.03).
Conclusions: In this large, national hospital-based registry study, adverse pathology was not significantly associated with poorer survival outcomes in patients with low-risk prostate cancer. These findings suggest an opportunity to further refine surrogates for AS candidacy.
Source of Funding: This work is supported in part by grants from the National Cancer Institute (P30CA072720) and generous support from the Marion and Norman Tanzman Charitable Foundation and Mr. Malcolm Wernik.
Methods: We queried the National Cancer Database to identify patients diagnosed with low-risk prostate cancer (Gleason score (GS) 6, clinical stage T1-T2a, and Prostate-Specific Antigen (PSA) <10 ng/mL), who underwent radical prostatectomy from 2004 to 2016. The primary objective was to compare OS between patients with adverse pathology, defined as pathological GS 7+ or pathological stage =T3 and/or N1, compared to those who did not. We used a Kaplan-Meier product limit estimate to determine five and ten-year OS and a log-rank test to compare OS. Adjusted Cox proportional hazard models were used to analyze the association between adverse pathology and survival. Additionally, we used multivariate logistic regression to evaluate pre-operative predictors of adverse pathology.
Results: Among low-risk patients treated with prostatectomy (N=72,274), 34,234 (47.4%) experienced pathologic upstage or upgrade. The majority, 83.2%, had pathological GS 7+ disease alone, while 16.7% had both pathological GS 7+ and pT3+/N1, and <0.1% had pT3+ or pN1+ alone. Lower age, White race, higher comorbidity score, lack of insurance, no high school diploma, treatment outside of a community cancer program, Midwest or South relative to Northeast region, and higher PSA were associated with adverse pathology (p <0.001). Five-year OS was 98.0% and 97.8%, while ten-year OS was 92.2% and 87.3% for patients with and without adverse pathology, respectively (Figure 1). On multivariate analysis, neither upstaging nor upgrading was significantly associated with worse OS compared to patients with organ-confined pathology (HR = 1.05, 95% CI = [0.95, 1.15], p = 0.03).
Conclusions: In this large, national hospital-based registry study, adverse pathology was not significantly associated with poorer survival outcomes in patients with low-risk prostate cancer. These findings suggest an opportunity to further refine surrogates for AS candidacy.
Source of Funding: This work is supported in part by grants from the National Cancer Institute (P30CA072720) and generous support from the Marion and Norman Tanzman Charitable Foundation and Mr. Malcolm Wernik.

.jpg)
.jpg)