Back
Poster, Podium & Video Sessions
Urodynamics/Lower Urinary Tract Dysfunction/Female Pelvic Medicine: Female Incontinence: Therapy I
PD06-01: Real World Outcomes of Urethral Injection of Polyacrylamide Hydrogel (Bulkamid&[reg]) for Stress Urinary Incontinence with Intrinsic Sphincter Deficiency, Prior Urethral Surgery, or Prior Mesh Sling Excision
Friday, May 13, 2022
9:30 AM – 9:40 AM
Location: Room 255
Justina Tam*, Hannah Koenig, Shreeya Popat, Deborah Sparks, Alvaro Lucioni, Kathleen Kobashi, Una Lee, Seattle, WA
- JT
Justina Tam, MD
Stony Brook Medicine
Podium Presenter(s)
Introduction: Polyacrylamide Hydrogel (PAHG) is a transurethral bulking agent with demonstrated safety, efficacy, and durability in the treatment of stress urinary incontinence (SUI). However, real world outcomes after mesh sling excision and/or refractory SUI have not been reported. The objective of this study is to examine PAHG treatment outcomes in women with intrinsic sphincter deficiency (ISD), prior SUI surgery, or mesh sling excision, i.e. those with “complex urethras.”
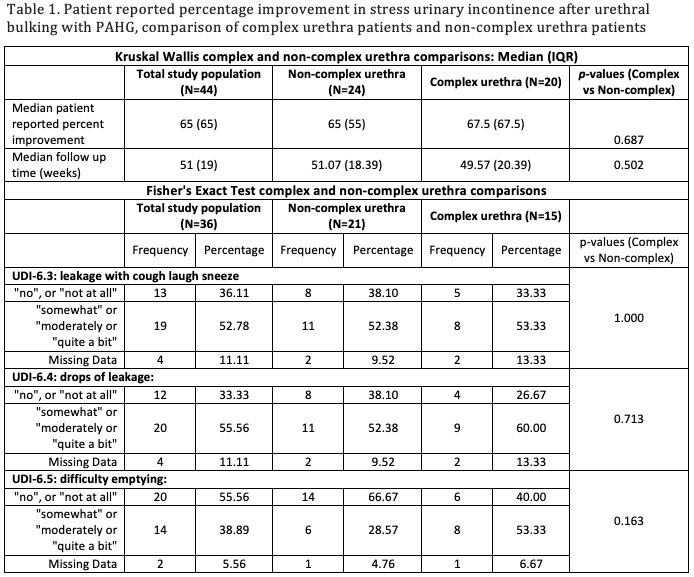
Methods: Pre- and post-procedural questionnaires from women undergoing urethral bulking with PAHG at a single institution with 3 FPMRS surgeons, including the Urogenital Distress Inventory-6 (UDI6), Pelvic Floor Impact Questionniare-7 (PFIQ-7), and postoperative patient reported percentage improvement were analyzed. Demographics and prior surgical procedures were collected. Complex urethra patients included women with SUI and ISD (Valsalva leak point pressure <60cmH20), pelvic radiation, prior mesh sling excision, and/or prior SUI surgery. Non-complex urethra patients had SUI without these factors. Patients were excluded from analysis if they received PAHG at the same time as another procedure or had a pelvic floor surgery after PAHG injection. Statistical analysis was performed using Kruskal-Wallis and Fisher’s Exact tests.
Results: From May 2020 to March 2021, 103 women with SUI received urethral bulking with PAHG. Of 64 women eligible for analysis (9 had 2 PAHG injections), with median age 53, 44 had follow-up data (20 with complex urethra and 24 with non-complex urethra). Median patient reported percentage improvement was 67.5% in complex urethras, and 65% in non-complex urethras, with median follow up time of 50 and 51 weeks in complex and non-complex urethras, respectively, with no statistical difference between the two groups (Table 1). There were no statistical differences between UDI-6 and PFIQ-7 questionnaire responses.
Conclusions: Despite a history of ISD, prior SUI surgery, prior mesh sling excision, or pelvic radiation, women with complex urethras achieved >65% patient reported improvement in SUI with PAHG at one year, similar to non-complex urethra patients who undergo PAHG for SUI in a real world setting.
Source of Funding: N/A
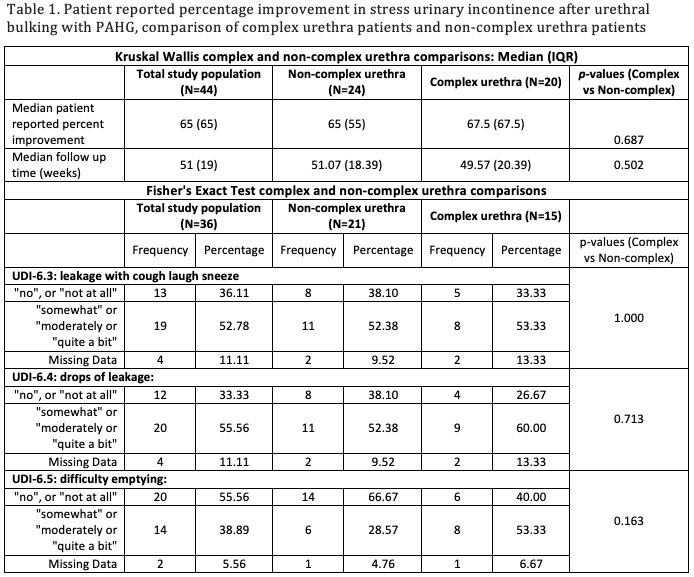
Methods: Pre- and post-procedural questionnaires from women undergoing urethral bulking with PAHG at a single institution with 3 FPMRS surgeons, including the Urogenital Distress Inventory-6 (UDI6), Pelvic Floor Impact Questionniare-7 (PFIQ-7), and postoperative patient reported percentage improvement were analyzed. Demographics and prior surgical procedures were collected. Complex urethra patients included women with SUI and ISD (Valsalva leak point pressure <60cmH20), pelvic radiation, prior mesh sling excision, and/or prior SUI surgery. Non-complex urethra patients had SUI without these factors. Patients were excluded from analysis if they received PAHG at the same time as another procedure or had a pelvic floor surgery after PAHG injection. Statistical analysis was performed using Kruskal-Wallis and Fisher’s Exact tests.
Results: From May 2020 to March 2021, 103 women with SUI received urethral bulking with PAHG. Of 64 women eligible for analysis (9 had 2 PAHG injections), with median age 53, 44 had follow-up data (20 with complex urethra and 24 with non-complex urethra). Median patient reported percentage improvement was 67.5% in complex urethras, and 65% in non-complex urethras, with median follow up time of 50 and 51 weeks in complex and non-complex urethras, respectively, with no statistical difference between the two groups (Table 1). There were no statistical differences between UDI-6 and PFIQ-7 questionnaire responses.
Conclusions: Despite a history of ISD, prior SUI surgery, prior mesh sling excision, or pelvic radiation, women with complex urethras achieved >65% patient reported improvement in SUI with PAHG at one year, similar to non-complex urethra patients who undergo PAHG for SUI in a real world setting.
Source of Funding: N/A

.jpg)
.jpg)