Back
Poster, Podium & Video Sessions
Podium
PD06: Urodynamics/Lower Urinary Tract Dysfunction/Female Pelvic Medicine: Female Incontinence: Therapy I
PD06-12: Usage and Cost of Urinary Incontinence Products in Women
Friday, May 13, 2022
11:20 AM – 11:30 AM
Location: Room 255
Leah Chisholm*, Elisabeth Sebesta, Stephanie Gleicher, Melissa Kaufman, Roger Dmochowski, W. Stuart Reynolds, Nashville, TN
- LC
Podium Presenter(s)
Introduction: Urinary incontinence (UI) is common in US women, who often use incontinence containment products to self-manage, the cost of which can be a great burden. Because few studies have sought to quantify use and costs of incontinence products associated with subtypes of incontinence and severity, therefore we aimed to quantify incontinence product use and personal costs to women.
Methods: This is a secondary analysis of a sample of 2,627 US adult women, recruited electronically via ResearchMatch. Participants were asked about daily numbers and types of incontinence products used and weekly costs. Urinary symptoms were assessed via LURN SI-10 and ICIQ-UI SF, along with demographic and baseline clinical information. Descriptive statistics were performed, in addition to Wilcoxon rank sum and Kruskal-Wallis tests to compare mean incontinence product usage based on type of incontinence, symptom severity, and other demographics.
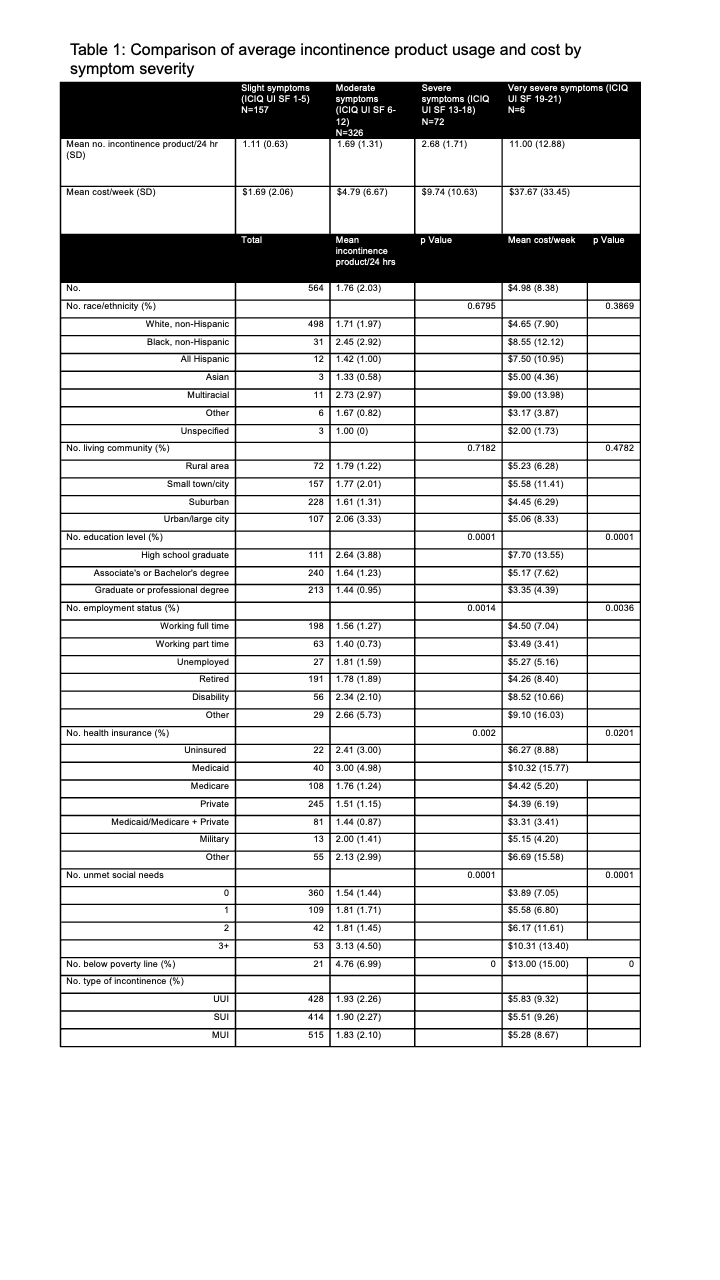
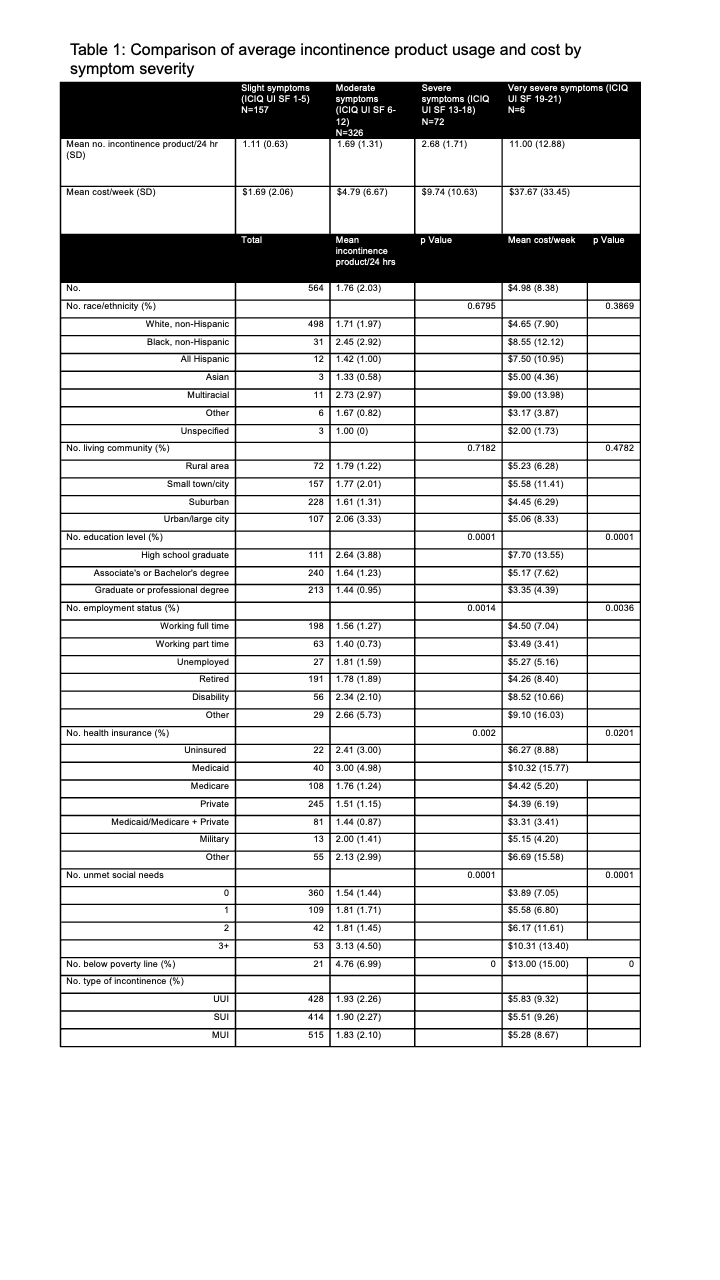
Results: A total of 1,522 of all women reported any weekly incontinence on ICIQ-UI SF (57.94%). The mean age of incontinent patients was 52.02 +/- 15.86 years, and the majority of patients identified as non-Hispanic white (86.60%). 564 patients (37.06%) reported using pads or diapers daily, with a mean of 1.6 +/- 1.5 (range 0 to 20) pads and a mean weekly cost of $4.98 +/- $8.38 (range $0 - $100). Usage or cost did not differ by type of UI, race, or living community. Usage and cost was more in women who had less than college education, on disability, used Medicaid or were uninsured, had 3 or more unmet social needs, or household income below the poverty line (all results in Table 1). Looking more closely at ICIQ-0UI SF, daily pad use and weekly costs increased with symptom severity, with the biggest increase between those with severe and very severe symptoms.
Conclusions: In this study of incontinent women, those with severe or very severe symptoms on ICIQ-UI SF reported using on average 3 to 11 pads/diapers per day, at a significant personal cost that averaged $10 to $38 weekly. For those with more unmet social needs, uninsured or using Medicaid, less than college education, lower income, and on disability, these costs were even greater, and may be prohibitive.
Source of Funding: UL1 TR000445 from NCATS/NIH
Methods: This is a secondary analysis of a sample of 2,627 US adult women, recruited electronically via ResearchMatch. Participants were asked about daily numbers and types of incontinence products used and weekly costs. Urinary symptoms were assessed via LURN SI-10 and ICIQ-UI SF, along with demographic and baseline clinical information. Descriptive statistics were performed, in addition to Wilcoxon rank sum and Kruskal-Wallis tests to compare mean incontinence product usage based on type of incontinence, symptom severity, and other demographics.
Results: A total of 1,522 of all women reported any weekly incontinence on ICIQ-UI SF (57.94%). The mean age of incontinent patients was 52.02 +/- 15.86 years, and the majority of patients identified as non-Hispanic white (86.60%). 564 patients (37.06%) reported using pads or diapers daily, with a mean of 1.6 +/- 1.5 (range 0 to 20) pads and a mean weekly cost of $4.98 +/- $8.38 (range $0 - $100). Usage or cost did not differ by type of UI, race, or living community. Usage and cost was more in women who had less than college education, on disability, used Medicaid or were uninsured, had 3 or more unmet social needs, or household income below the poverty line (all results in Table 1). Looking more closely at ICIQ-0UI SF, daily pad use and weekly costs increased with symptom severity, with the biggest increase between those with severe and very severe symptoms.
Conclusions: In this study of incontinent women, those with severe or very severe symptoms on ICIQ-UI SF reported using on average 3 to 11 pads/diapers per day, at a significant personal cost that averaged $10 to $38 weekly. For those with more unmet social needs, uninsured or using Medicaid, less than college education, lower income, and on disability, these costs were even greater, and may be prohibitive.
Source of Funding: UL1 TR000445 from NCATS/NIH

.jpg)
.jpg)