Podium
PD08: Infections/Inflammation/Cystic Disease of the Genitourinary Tract: Interstitial Cystitis
-

Bradley Erickson, MD, MS
Professor
University of Iowa
Podium Presenter(s)
Introduction: Inter- and intra-day fluctuation in pelvic pain in patients with UCPPS is poorly understood. This study deployed a mobile phone application (mAPP) to assess ecological momentary assessments of pelvic pain. We hypothesized that 1) variations in pain severity, trajectory and stability would cluster into distinct phenotypes and 2) these clusters would be associated with quality of life (QOL) and illness impact (II) metrics.
Methods: A previously validated mAPP was provided to UCPPS patients enrolled in the Multidisciplinary Approach to Chronic Pelvic Pain Symptoms Pattern Study (MAPP II SPS) following a 6-month in-clinic visit. Notifications were sent to each mAPP participant 4-times daily for 14 consecutive days (t=56 sampling points) asking about the presence/severity of pelvic pain (PP). A functional mixed effects clustering algorithm in which subgroups are clustered both in terms of group-average trajectories and within-group variabilities, was applied to patient PP trajectories. Associations between demographic, urinary urgency, pain severity, QOL and II measures obtained at 6 months and functional cluster membership were estimated, adjusting for baseline PP severity.
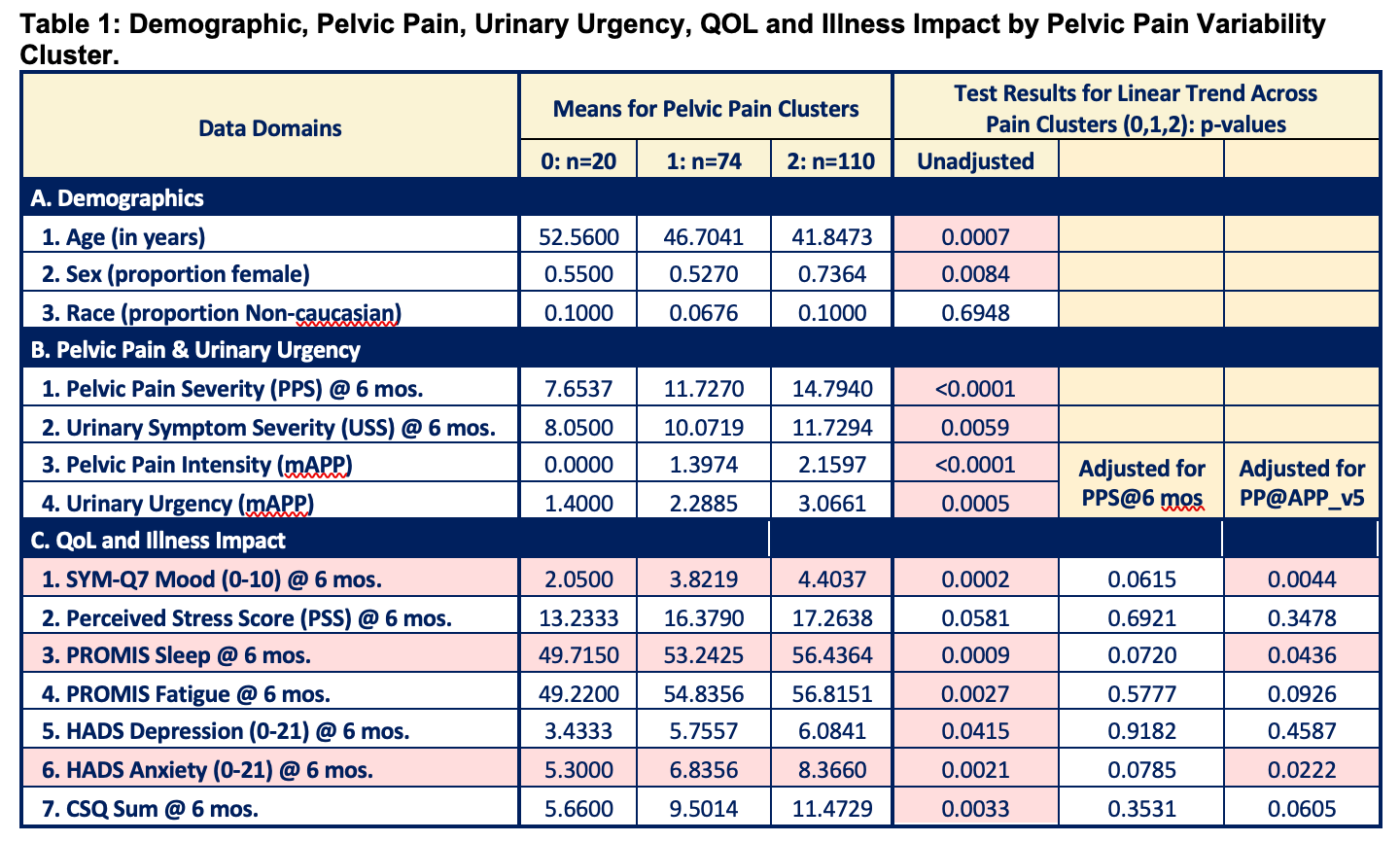
Results: Longitudinal PP severity data from n=204 patients were utilized to generate K=3 PP clusters (Figure 1), that can be characterized as 1) no variability (NV, n=20); 2) low variability (LV, n=74); and 3) high variability (HV, n=110). Significant differences in clusters were noted (Table 1), with patients in the HV cluster being younger, more likely to be female, have higher baseline pain and urgency scores, report worse QOL and higher II versus NV and LV clusters.
Conclusions: A 14-day study that assessed inter- and intra-day pain variability identified three distinct UCPPS PP clusters that differ significantly by demographics, baseline pain/urgency, QOL and II. Subjects with the highest variability had worse sleep, decreased mood and more anxiety relative to those with more stable pain scores.
Source of Funding: NIH/NIDDK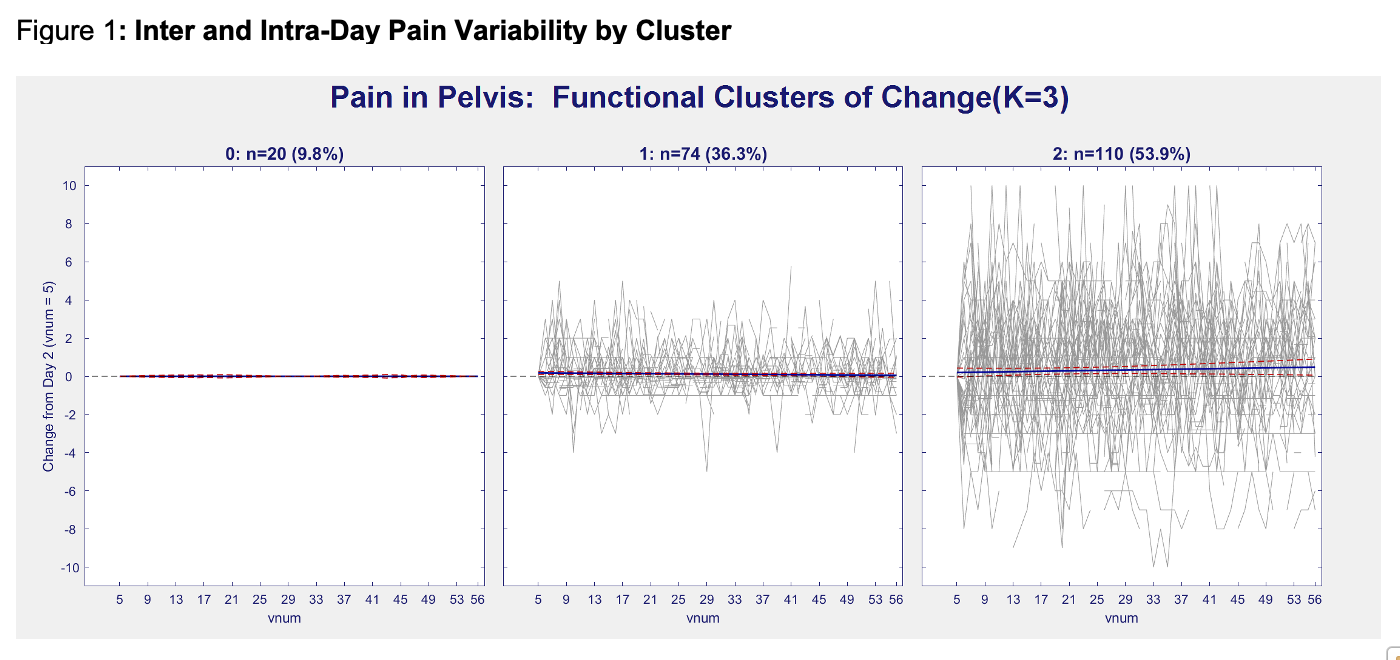

.jpg)
.jpg)