Back
Poster, Podium & Video Sessions
Podium
PD09: Infertility: Epidemiology & Evaluation I
PD09-11: Vein diameter on ultrasound as predictor of semen parameter improvement after varicocelectomy
Friday, May 13, 2022
2:40 PM – 2:50 PM
Location: Room 252
Leon Telis*, Alan Paniagua Cruz, Kirolos Meilika, New York, NY, Hira Chaudhry, Philadelphia, PA, Michael Huaman, Brooklyn, NY, Boback M. Berookhim, New York, NY

Leon Telis, MD
Northwell Health
Podium Presenter(s)
Introduction: Clinical presence and grade of varicocele has been associated with the degree of spermatogenic response to varicocelectomy. There have been no objective pre-operative factors that have been found to correlate with spermatogenic improvement post-varicocelectomy. We aim to determine whether preoperative venous diameter on ultrasound may predict semen parameter improvement post-varicocelectomy.
Methods: We performed a retrospective chart review of a single-surgeon cohort of patients undergoing microsurgical varicocelectomy to assess the impact of pre-operative ultrasound varicocele diameter on changes in semen analysis. Sonography was performed at local centers with experience in scrotal Doppler sonography. Maximal internal spermatic vein diameters were reported. Paired t-test and Wilcoxon signed-rank test were used to analyze changes in pre- and post-operative semen parameters. Paired t-test was used to further analyze changes in pre- and post-operative semen parameters among unilateral vs bilateral varicocelectomy. Statistical significance was defined as p<0.05. Kendall rank coefficient was performed to assess correlation of varicocele clinical grade and vein diameter on ultrasound.
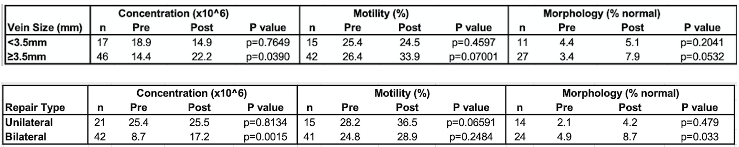
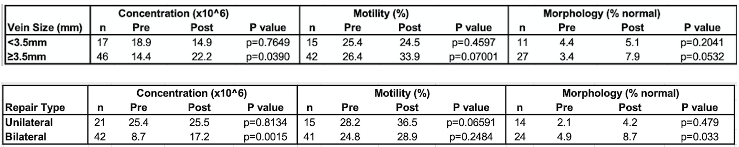
Results: The last 180 consecutive patients who underwent subinguinal microsurgical varicocelectomy were evaluated. Median age of patients was 32 years (range 19-57). 56 patients with available post-operative semen analyses underwent bilateral repair and 49 patients underwent unilateral repair. Mean time from surgery to post-operative semen analysis was 5.4 months. Men who underwent varicocelectomy with vein diameter >3.5 mm had a significant improvement in sperm concentration. Improvement in sperm motility and morphology was also noted in this cohort and approached statistical significance. Those with varicoceles <3.5 mm did not demonstrate an improvement in semen parameters. Significant improvement in semen concentration and morphology was noted among patients undergoing bilateral repair. There was a statistically significant association between clinical and radiographic varicocele size (tau = 0.391, p<0.001).
Conclusions: We identified an improvement in semen analysis parameters after varicocele repair in men with clinical varicoceles with venous diameter >3.5mm on ultrasound.
Source of Funding: None
Methods: We performed a retrospective chart review of a single-surgeon cohort of patients undergoing microsurgical varicocelectomy to assess the impact of pre-operative ultrasound varicocele diameter on changes in semen analysis. Sonography was performed at local centers with experience in scrotal Doppler sonography. Maximal internal spermatic vein diameters were reported. Paired t-test and Wilcoxon signed-rank test were used to analyze changes in pre- and post-operative semen parameters. Paired t-test was used to further analyze changes in pre- and post-operative semen parameters among unilateral vs bilateral varicocelectomy. Statistical significance was defined as p<0.05. Kendall rank coefficient was performed to assess correlation of varicocele clinical grade and vein diameter on ultrasound.
Results: The last 180 consecutive patients who underwent subinguinal microsurgical varicocelectomy were evaluated. Median age of patients was 32 years (range 19-57). 56 patients with available post-operative semen analyses underwent bilateral repair and 49 patients underwent unilateral repair. Mean time from surgery to post-operative semen analysis was 5.4 months. Men who underwent varicocelectomy with vein diameter >3.5 mm had a significant improvement in sperm concentration. Improvement in sperm motility and morphology was also noted in this cohort and approached statistical significance. Those with varicoceles <3.5 mm did not demonstrate an improvement in semen parameters. Significant improvement in semen concentration and morphology was noted among patients undergoing bilateral repair. There was a statistically significant association between clinical and radiographic varicocele size (tau = 0.391, p<0.001).
Conclusions: We identified an improvement in semen analysis parameters after varicocele repair in men with clinical varicoceles with venous diameter >3.5mm on ultrasound.
Source of Funding: None

.jpg)
.jpg)