Back
Poster, Podium & Video Sessions
Podium
PD11: Prostate Cancer: Detection & Screening II
PD11-04: The Limited Utility of Prostate Health Index in African American Men with a PSA 4-10
Friday, May 13, 2022
1:30 PM – 1:40 PM
Location: Room 245
Kostantinos Morris*, Judd Moul, Srinath Kotamarti, Durham, NC

Kostantinos Morris, MD
Indiana University
Podium Presenter(s)
Introduction: Prostate Health Index (PHI) is a blood test approved for men being evaluated for prostate cancer (PCa) with a prostate specific antigen (PSA) in the “gray zone” of 4-10 ng/ml. As such, in the largest examination of PHI in African American (AA) men, we sought to assess PHI utility in the pre-biopsy work-up of this demographic, who notably were minimally represented in the original validation studies.
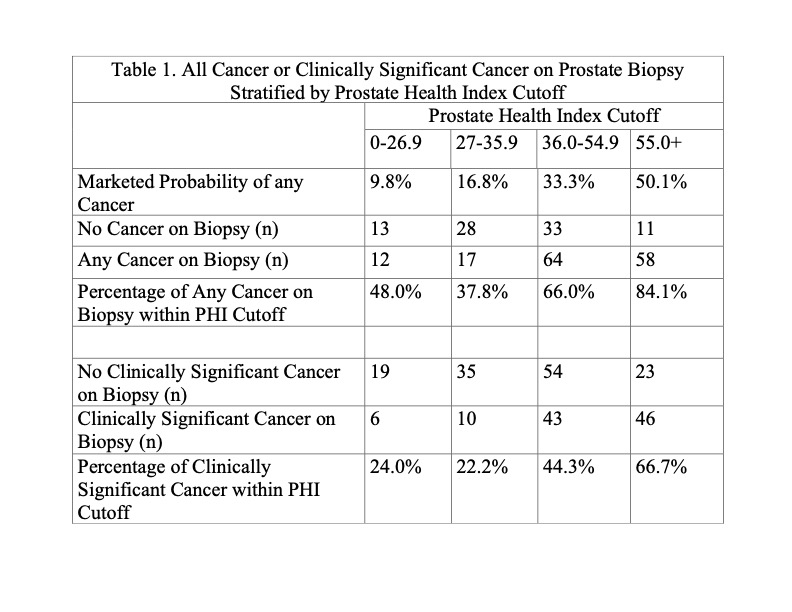
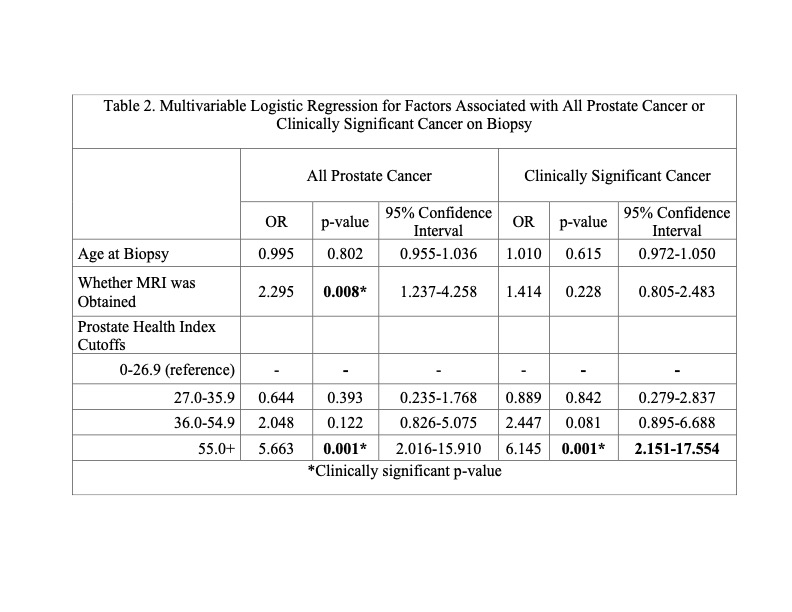
Methods: AA men in the Duke Health System with a PSA of 4-10 ng/mL, a PHI score, and subsequent prostate biopsy between 2016-2020 were identified. Established PHI cutoffs were utilized to stratify patients (Table 1). Multivariable logistical regressions were performed to assess possible predictors of cancer detection with the lowest PHI cutoff serving as reference. Clinically significant cancer (CSC) was defined as Gleason =7.
Results: A total of 1,131 AA men underwent PHI testing, and 236 met final inclusion criteria. Average age was 61.2 years. Mean PSA and PHI for the entire cohort were 6.5 ng/ml (SD 1.7) and 48.5 (SD 21.6), respectively. Detection rate at biopsy was 64.0% (n=151) for any PCa, ranging from 48.0% for PHI 0-26.9 to 84.1% for PHI =55 (Table 1). For CSC, overall detection rate was 44.5% (n=105), ranging from 24.0% for PHI 0-26.9 to 66.7% for PHI =55 (Table 1). On multivariable analysis, PHI =55 cutoff was the only PHI category associated with identification of all PCa (OR 5.66, p<0.01) and CSC (OR 6.15, p<0.01) (Table 2).
Conclusions: Two-thirds of patients in the highest PHI category (= 55) were found to have CSC. This cutoff was the only stratification significantly associated with PCa detection. However, alarmingly, all established PHI cutoffs featured high rates of PCa and CSC. While elevated PHI in AA men with equivocal PSA should be regarded with heightened suspicion, our findings also highlight the difficulty in identifying patients at low risk who may benefit from a less fastidious approach. Likely, the current established stratification for PHI needs to be re-evaluated for the high-risk cohort of AA men.
Source of Funding: None
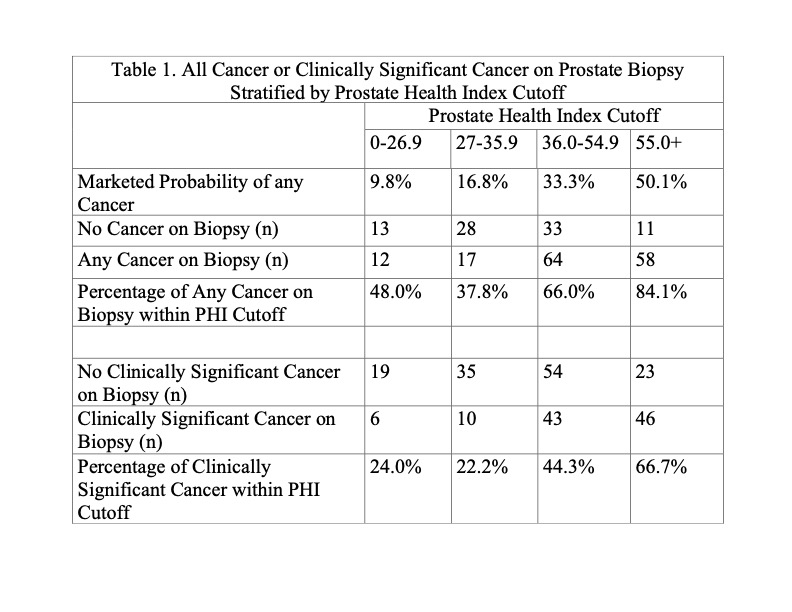
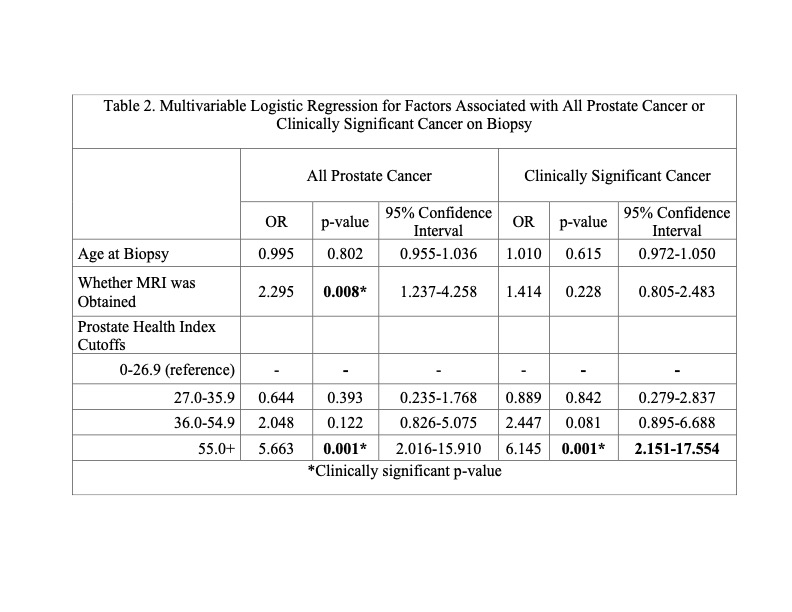
Methods: AA men in the Duke Health System with a PSA of 4-10 ng/mL, a PHI score, and subsequent prostate biopsy between 2016-2020 were identified. Established PHI cutoffs were utilized to stratify patients (Table 1). Multivariable logistical regressions were performed to assess possible predictors of cancer detection with the lowest PHI cutoff serving as reference. Clinically significant cancer (CSC) was defined as Gleason =7.
Results: A total of 1,131 AA men underwent PHI testing, and 236 met final inclusion criteria. Average age was 61.2 years. Mean PSA and PHI for the entire cohort were 6.5 ng/ml (SD 1.7) and 48.5 (SD 21.6), respectively. Detection rate at biopsy was 64.0% (n=151) for any PCa, ranging from 48.0% for PHI 0-26.9 to 84.1% for PHI =55 (Table 1). For CSC, overall detection rate was 44.5% (n=105), ranging from 24.0% for PHI 0-26.9 to 66.7% for PHI =55 (Table 1). On multivariable analysis, PHI =55 cutoff was the only PHI category associated with identification of all PCa (OR 5.66, p<0.01) and CSC (OR 6.15, p<0.01) (Table 2).
Conclusions: Two-thirds of patients in the highest PHI category (= 55) were found to have CSC. This cutoff was the only stratification significantly associated with PCa detection. However, alarmingly, all established PHI cutoffs featured high rates of PCa and CSC. While elevated PHI in AA men with equivocal PSA should be regarded with heightened suspicion, our findings also highlight the difficulty in identifying patients at low risk who may benefit from a less fastidious approach. Likely, the current established stratification for PHI needs to be re-evaluated for the high-risk cohort of AA men.
Source of Funding: None

.jpg)
.jpg)