Back
Poster, Podium & Video Sessions
Bladder Cancer: Basic Research & Pathophysiology II
PD12-01: Bladder Tumor Microbiome May Augment Response to BCG in Non-Muscle Invasive Bladder Cancer
Friday, May 13, 2022
1:00 PM – 1:10 PM
Location: Room 244
Jacob Knorr*, Glenn Werneburg, Ava Adler, Jose Agudelo, Prithvi Murthy, Rebecca Campbell, Petar Bajic, Nima Almassi, Christopher Weight, Georges-Pascal Haber, Aaron Miller, Byron Lee, CLEVELAND, OH
- JK
Jacob Knorr, BS
Cleveland Clinic
Podium Presenter(s)
Introduction: Despite proven efficacy and longstanding use of Mycobacterium bovis Bacillus Calmette-Guerin (BCG) for non-muscle invasive bladder cancer, it remains unclear which patients respond to treatment. A potential determinant may be the urinary microbiome, which is closely tied to the host immune system and implicated in genitourinary disease. We sought to investigate commensal microbial associations with BCG responder versus non-responder status in tumors from bladder cancer patients, and identify possible mechanisms for commensal interaction in the BCG response.
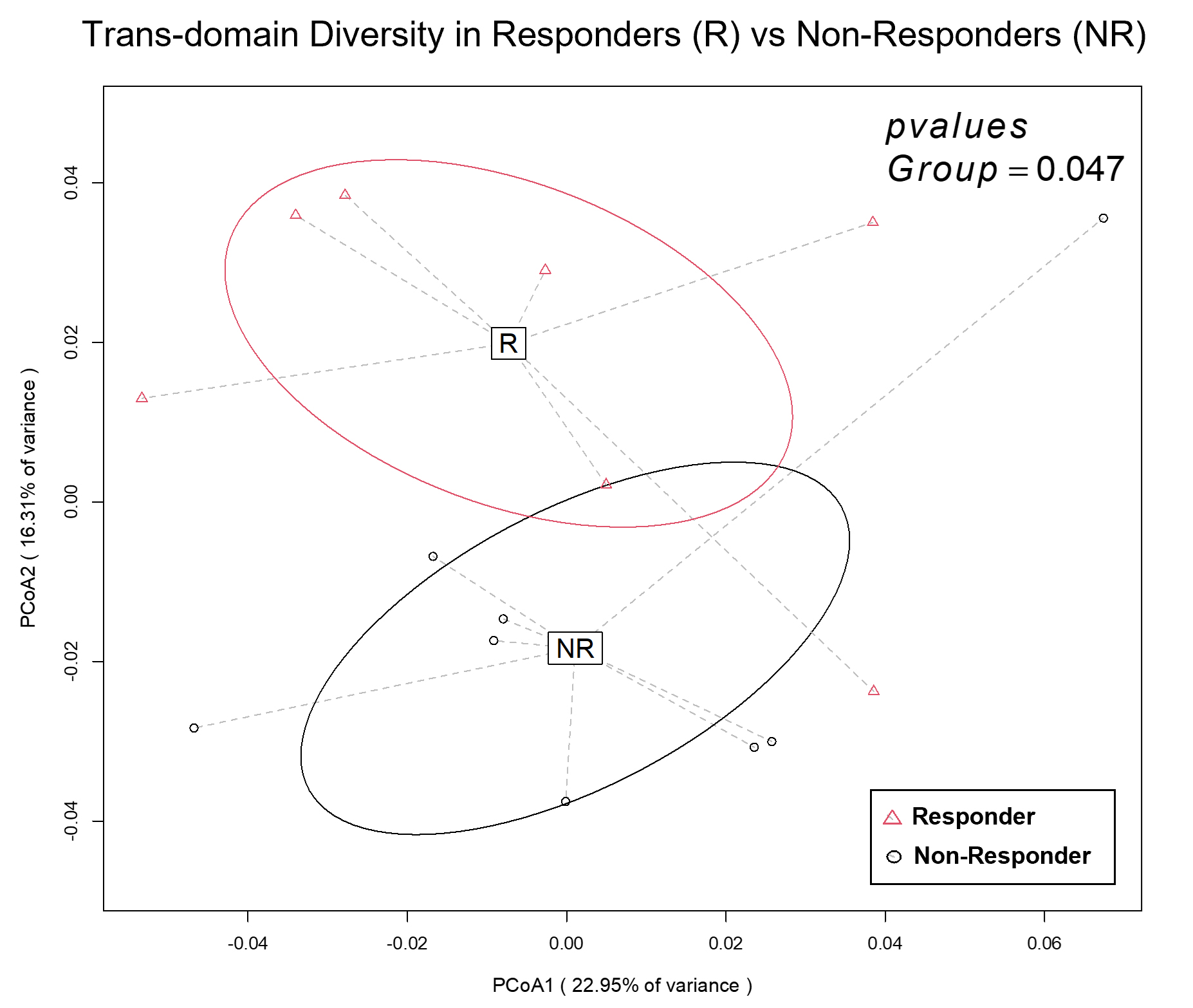
Methods: 16S next-generation sequencing (NGS) and shotgun metagenomics were performed on formalin-fixed bladder tumor tissue from patients prior to intravesical BCG therapy for bladder cancer. Sequence reads were assigned to genus-level amplicon sequence variants (ASVs) in DADA2 and analyzed in Phyloseq. To determine microbial influences on BCG internalization, GFP-tagged BCG was co-cultured with a urothelial carcinoma (UCC) cell line and a series of candidate microbial species. BCG response was defined as no disease two years from induction BCG. Differences between BCG responders and non-responders were assessed using t-tests, Permanova, and principal components analyses.
Results: 47 patients (23 responders, 24 non-responders) were included in analysis. Overall microbiome composition differed significantly as determined independently by NGS (p=0.042) and shotgun metagenomics (p = 0.047, Figure). Lactobacillus spp were enriched in BCG responders, and Corynebacterium spp were enriched in BCG non-responders. Species richness was not significantly different between BCG responders and non-responders (p=0.053). BCG-GFP internalization by UCCs was significantly greater when co-cultured with Lactobacillus crispatus (197/1156, 17%) compared to controls (160/1490, 10.7%) (p=0.0001).
Conclusions: There is a robust and consistent compositional difference in the urinary microbiome between BCG responders and non-responders. Lactobacillus crispatus was associated with significantly increased BCG internalization. These findings suggest the urinary tumor microbiome is associated with response status and may directly augment BCG response, opening new avenues for investigations to optimize bladder-sparing therapy in bladder cancer.
Source of Funding: CWRU CCCC
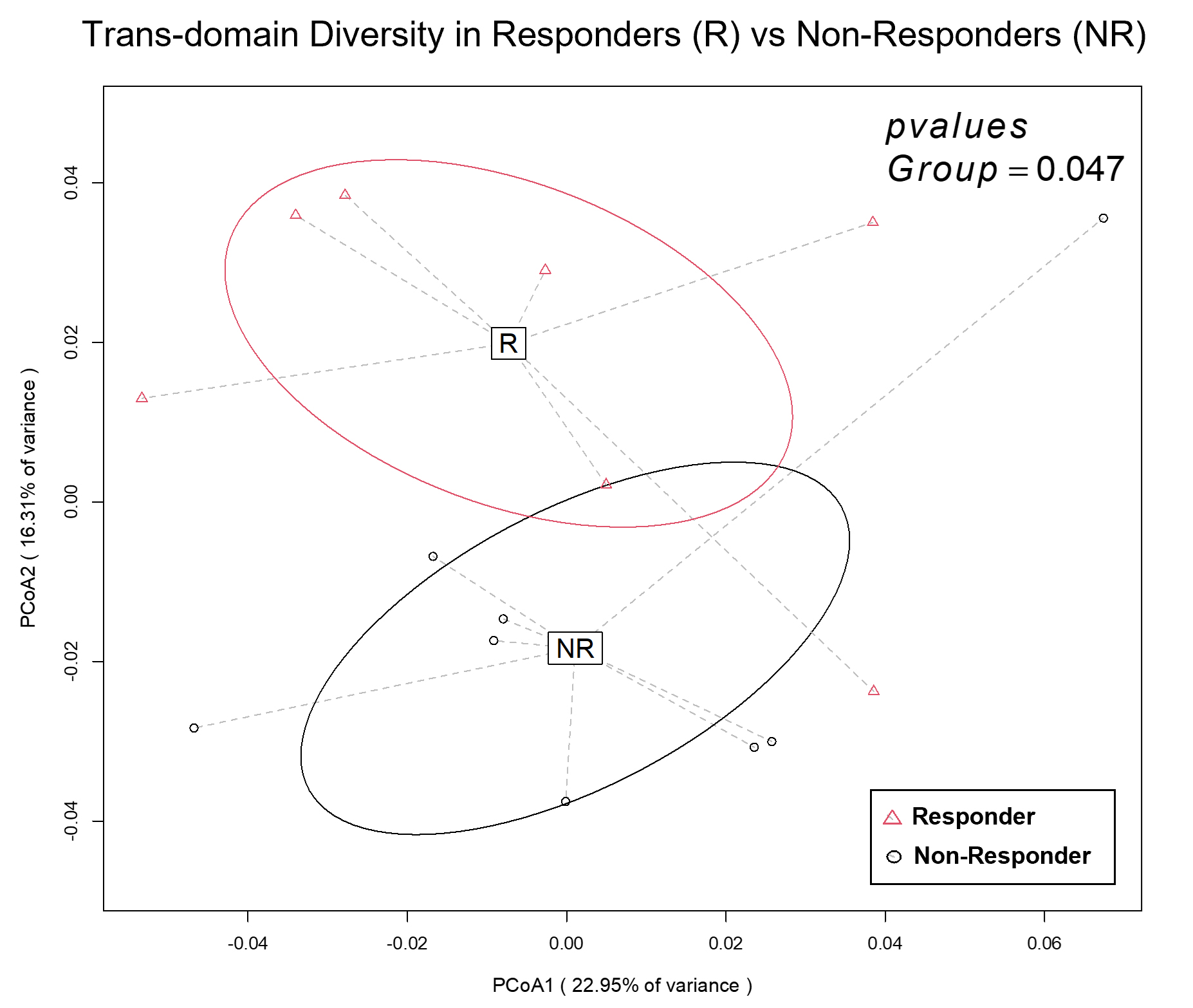
Methods: 16S next-generation sequencing (NGS) and shotgun metagenomics were performed on formalin-fixed bladder tumor tissue from patients prior to intravesical BCG therapy for bladder cancer. Sequence reads were assigned to genus-level amplicon sequence variants (ASVs) in DADA2 and analyzed in Phyloseq. To determine microbial influences on BCG internalization, GFP-tagged BCG was co-cultured with a urothelial carcinoma (UCC) cell line and a series of candidate microbial species. BCG response was defined as no disease two years from induction BCG. Differences between BCG responders and non-responders were assessed using t-tests, Permanova, and principal components analyses.
Results: 47 patients (23 responders, 24 non-responders) were included in analysis. Overall microbiome composition differed significantly as determined independently by NGS (p=0.042) and shotgun metagenomics (p = 0.047, Figure). Lactobacillus spp were enriched in BCG responders, and Corynebacterium spp were enriched in BCG non-responders. Species richness was not significantly different between BCG responders and non-responders (p=0.053). BCG-GFP internalization by UCCs was significantly greater when co-cultured with Lactobacillus crispatus (197/1156, 17%) compared to controls (160/1490, 10.7%) (p=0.0001).
Conclusions: There is a robust and consistent compositional difference in the urinary microbiome between BCG responders and non-responders. Lactobacillus crispatus was associated with significantly increased BCG internalization. These findings suggest the urinary tumor microbiome is associated with response status and may directly augment BCG response, opening new avenues for investigations to optimize bladder-sparing therapy in bladder cancer.
Source of Funding: CWRU CCCC

.jpg)
.jpg)