Back
Poster, Podium & Video Sessions
Podium
PD13: Prostate Cancer: Epidemiology & Natural History II
PD13-07: Cost-effectiveness Analysis of Arterial Catheter Insertion on Robotic-Assisted Laparoscopic Prostatectomy
Friday, May 13, 2022
4:30 PM – 4:40 PM
Location: Room 252
Rogelio Valdez*, Cleveland, OH, Johnathan Drevik, Philadelphia, PA, Ilaha Isali, Cleveland, OH, Alexander Kutikov, Philadelphia, PA, Mohit Sindhani, Delhi, India, Megan Prunty, Adam Calaway, Lee Ponsky, Cleveland, OH, Alberto Castro Bigalli, Laura Bukavina, Philadelphia, PA
Podium Presenter(s)
Introduction: As prostatectomy has transitioned from open surgery to robotic assisted and is now moving towards same day surgery in some areas the need for invasive monitoring has yet to be addressed. Here we evaluate the utility, outcomes, and cost of A-line placement in a single institution cohort for patients undergoing RALP.
Methods: A retrospective chart review was performed at a large tertiary care institution from July 2018 through January 2021. Hospital costs and cost effective analysis were performed on patients with A-line placement. Means with standard deviations were used to report continuous variables, while numbers and percentages were utilized to describe categorical variables. T-tests and Chi-square tests were used to compare categorical and continuous variables across study variables, respectively. Multivariable analyses were used to examine the association between A-line placement and the outcomes as mentioned above adjusting for the other co-variables
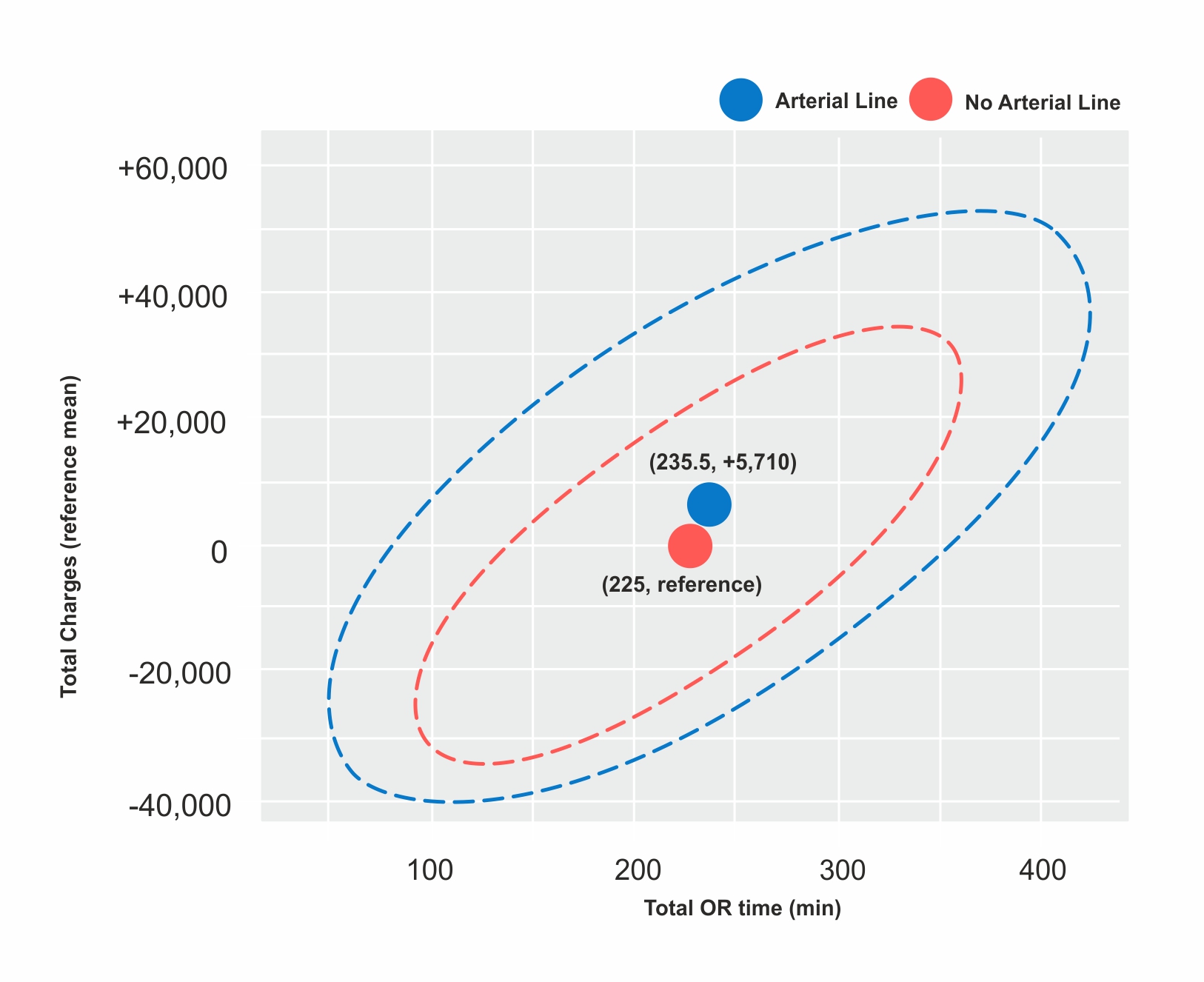
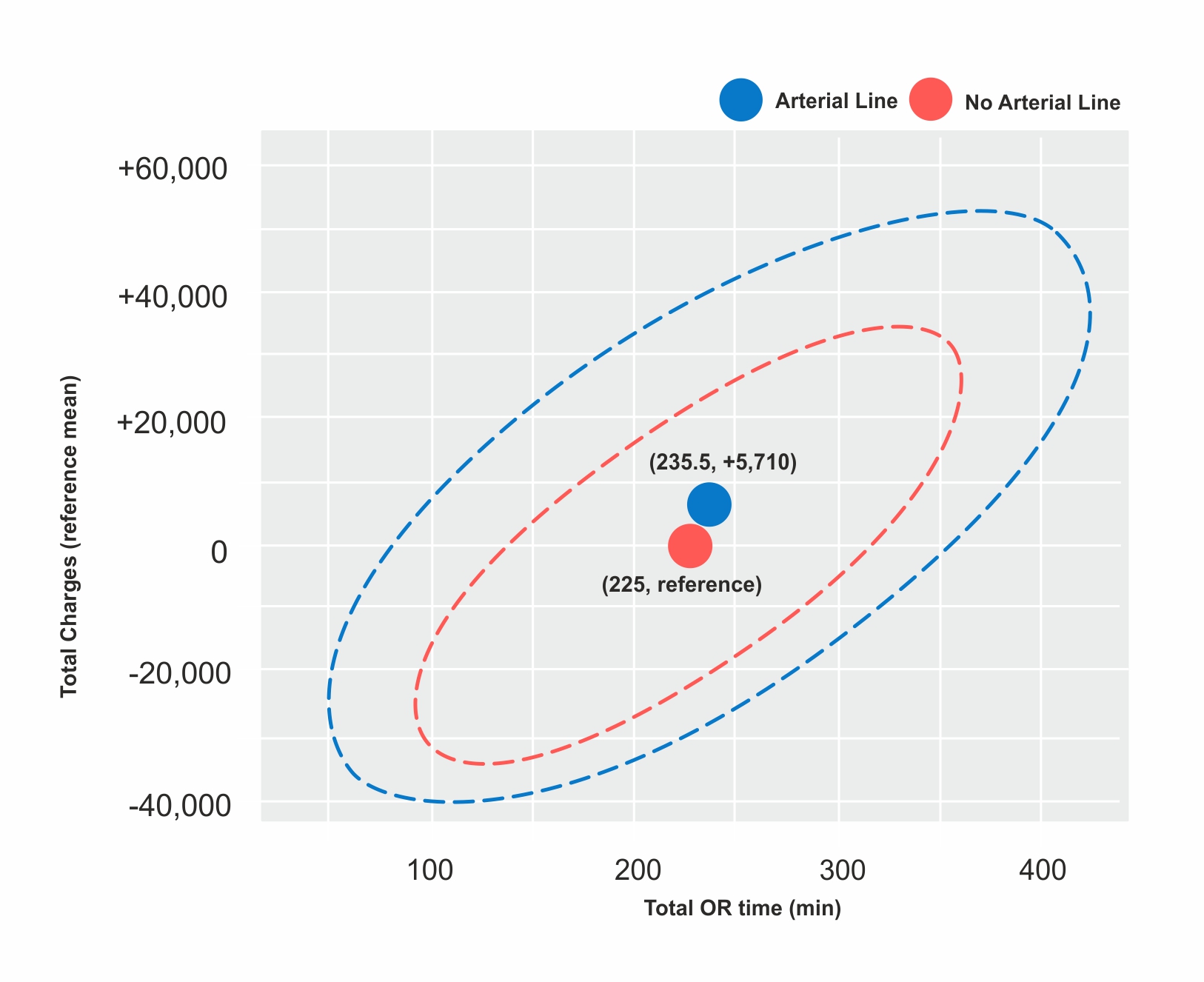
Results: In this patient cohort 296 patients were included of which 138 (46.6%) had A-lines placed. Patients with A-line placement were more likely to receive a higher volume of intra-operative crystalloid fluid resuscitation (2.1L vs. 1.8L, p< 0.01), and albumin (103.95 vs 59.12, p =0.06), as well as experienced a slightly increased length of stay (1.72 vs 1.31, p=0.02) The results also revealed an increase in total charges (A-line +5,710, p<0.001), total direct costs (A-line +395, p=0.004) and variable costs (A-line +389, p=0.004). While placement of arterial line while clinically increased total charges, total direct and variable costs, this was not significant (p=0.06) after adjusting for patient factorsOn our probabilistic modeling via Monte Carlo 1000 iterations, evaluating variance in total charges based on operative time and arterial line placement, showed an increase of total of 10.5 minutes in operative duration(min), and an increased total charge to the patient (5,710$). (fig)
Conclusions: While the use of A-lines was common in RRP, this practice is relatively antiquated and likely no longer useful in monitoring patients undergoing RALP. Use of A-lines is associated with higher costs to patients and hospitals, longer LOS, and no difference in operative outcomes.
Source of Funding: N/A
Methods: A retrospective chart review was performed at a large tertiary care institution from July 2018 through January 2021. Hospital costs and cost effective analysis were performed on patients with A-line placement. Means with standard deviations were used to report continuous variables, while numbers and percentages were utilized to describe categorical variables. T-tests and Chi-square tests were used to compare categorical and continuous variables across study variables, respectively. Multivariable analyses were used to examine the association between A-line placement and the outcomes as mentioned above adjusting for the other co-variables
Results: In this patient cohort 296 patients were included of which 138 (46.6%) had A-lines placed. Patients with A-line placement were more likely to receive a higher volume of intra-operative crystalloid fluid resuscitation (2.1L vs. 1.8L, p< 0.01), and albumin (103.95 vs 59.12, p =0.06), as well as experienced a slightly increased length of stay (1.72 vs 1.31, p=0.02) The results also revealed an increase in total charges (A-line +5,710, p<0.001), total direct costs (A-line +395, p=0.004) and variable costs (A-line +389, p=0.004). While placement of arterial line while clinically increased total charges, total direct and variable costs, this was not significant (p=0.06) after adjusting for patient factorsOn our probabilistic modeling via Monte Carlo 1000 iterations, evaluating variance in total charges based on operative time and arterial line placement, showed an increase of total of 10.5 minutes in operative duration(min), and an increased total charge to the patient (5,710$). (fig)
Conclusions: While the use of A-lines was common in RRP, this practice is relatively antiquated and likely no longer useful in monitoring patients undergoing RALP. Use of A-lines is associated with higher costs to patients and hospitals, longer LOS, and no difference in operative outcomes.
Source of Funding: N/A

.jpg)
.jpg)
.jpeg.jpg)