Back
Poster, Podium & Video Sessions
Podium
PD13: Prostate Cancer: Epidemiology & Natural History II
PD13-11: Disease trajectories and outcomes for men with castration resistant prostate cancer by use of nation-wide population-based observational data
Friday, May 13, 2022
5:10 PM – 5:20 PM
Location: Room 252
Eugenio Ventimiglia*, Milan, Italy, Anna Bill-Axelson, Uppsala, Sweden, Markus Aly, Gothenburg, Sweden, Martin Eklund, Stokholm, Sweden, Par Stattin, Hans Garmo, Uppsala, Sweden
- EV
Podium Presenter(s)
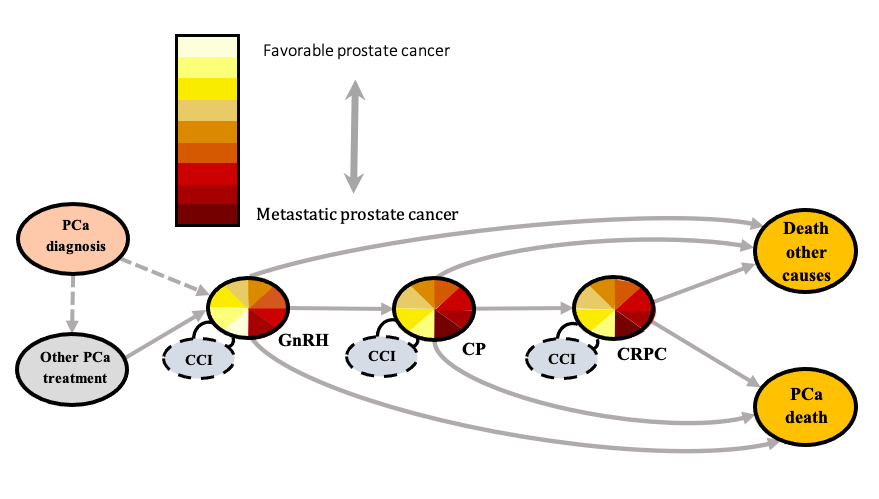
Introduction: Disease trajectories and outcomes for men with castration resistant prostate cancer (CRPC) are not known. We present here a state transition model which aims to describe disease trajectories around the CPRC state and to estimate CRPC state duration and survival outcomes.
Methods: We developed and applied a state-transition model based on population-based PSA data from 40% of the Swedish male adult population, which were linked to nationwide population-based databases to obtain complete data regarding prostate cancer (PCa) risk category, age, comorbidities, received treatments and drug prescriptions (n=28,394 men). The date of CRPC was defined for men in the state based on an increase in PSA, either first date of doubling of nadir PSA value with the last value higher than 2 ng/mL, or an absolute increase of 5 ng/mL or more whichever came first. Men with CRPC were classified into 8 different risk categories according to PSA at CRPC and to PSA doubling time. Using our model, we extracted and compared observed and predicted cumulative incidence of transitions to and from the CRPC state. Finally, we estimated the time spent in the CPRC state as well as the proportion of men who died of PCa during follow-up according to CRPC risk category.
Results: The state transition model, including states, treatment trajectories and transition probabilities around the CPRC state is shown in Figure 1. The predicted time spent in the CRPC state during the first 10 years after androgen deprivation therapy start varied from 1.1 years for the highest risk category to 3.9 years for the lowest risk category. The proportion on men who died of PCa within 10 years ranged from 93% for the highest risk category to 54% for lowest risk category.
Conclusions: Time spent in the CRPC state varied considerably in our cohort according to risk category, and most of the men with CRPC will eventually die from PCa. There was a good agreement between model estimates and observed data, showing that our model can accurately predict both CRPC duration and survival.
Source of Funding: none
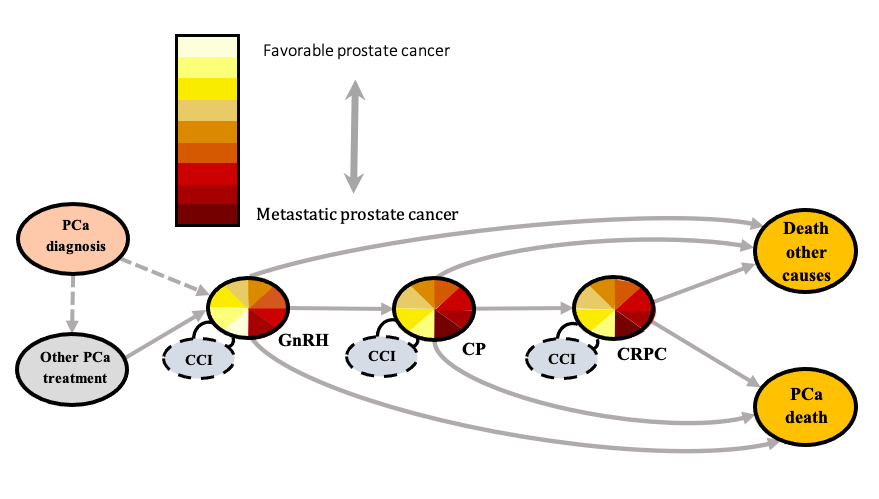
Methods: We developed and applied a state-transition model based on population-based PSA data from 40% of the Swedish male adult population, which were linked to nationwide population-based databases to obtain complete data regarding prostate cancer (PCa) risk category, age, comorbidities, received treatments and drug prescriptions (n=28,394 men). The date of CRPC was defined for men in the state based on an increase in PSA, either first date of doubling of nadir PSA value with the last value higher than 2 ng/mL, or an absolute increase of 5 ng/mL or more whichever came first. Men with CRPC were classified into 8 different risk categories according to PSA at CRPC and to PSA doubling time. Using our model, we extracted and compared observed and predicted cumulative incidence of transitions to and from the CRPC state. Finally, we estimated the time spent in the CPRC state as well as the proportion of men who died of PCa during follow-up according to CRPC risk category.
Results: The state transition model, including states, treatment trajectories and transition probabilities around the CPRC state is shown in Figure 1. The predicted time spent in the CRPC state during the first 10 years after androgen deprivation therapy start varied from 1.1 years for the highest risk category to 3.9 years for the lowest risk category. The proportion on men who died of PCa within 10 years ranged from 93% for the highest risk category to 54% for lowest risk category.
Conclusions: Time spent in the CRPC state varied considerably in our cohort according to risk category, and most of the men with CRPC will eventually die from PCa. There was a good agreement between model estimates and observed data, showing that our model can accurately predict both CRPC duration and survival.
Source of Funding: none

.jpg)
.jpg)