Back
Poster, Podium & Video Sessions
Podium
PD14: Bladder Cancer: Epidemiology & Evaluation I
PD14-10: Prospective Evaluation of a Comprehensive Geriatric Assessment (CGA) in Multidisciplinary Bladder Cancer Care: Feasibility and Impact on Decisional Conflict
Friday, May 13, 2022
5:00 PM – 5:10 PM
Location: Room 255
Sarah Psutka*, John Gore, Sarah Holt, Erin Dwyer, George Schade, Petros Grivas, Andrew Hsieh, John Lee, R. Bruce Montgomery, Michael Schweizer, Todd Yezefski, Evan Yu, Jonathan Chen, Jay Liao, Emily Weg, Jing Zeng, Tristan Alving, Samia Jannat, Jonathan Wright, Seattle, WA

Sarah P. Psutka, MD, MS (she/her/hers)
Associate Professor
University of Washington, Fred Hutchinson Cancer Center
Podium Presenter(s)
Introduction: Current guidelines recommend use of a CGA to quantify relevant vulnerabilities in older (> 65 years) patients prior to treatment selection. Our objective was to prospectively evaluate CGA in our Bladder Cancer Multidisciplinary Clinic (BCMC).
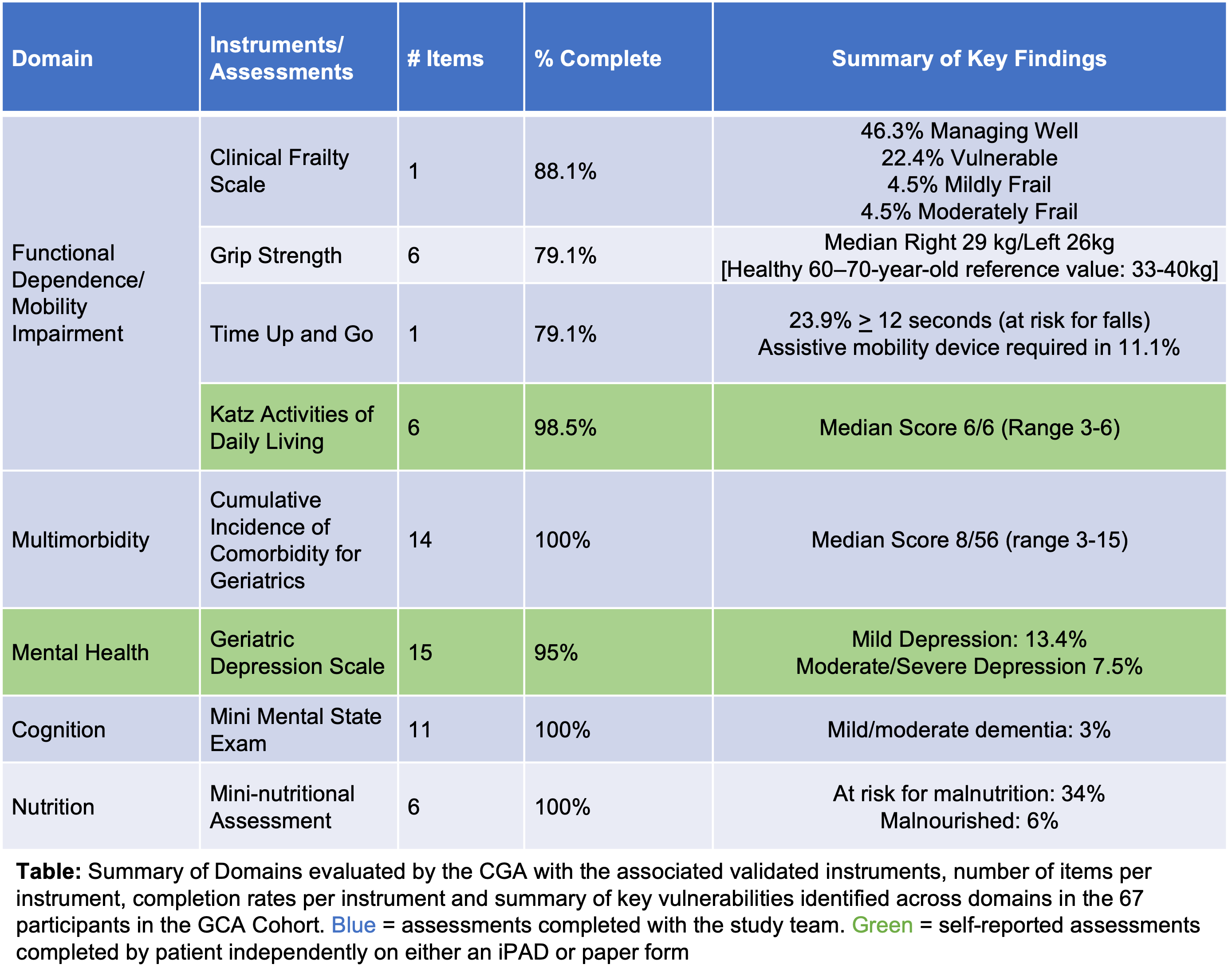
Methods: Patients seen in BCMC were prospectively enrolled from 6/1/20 to 7/20/21. In the first 3 months, participants underwent routine risk stratification (“Routine cohort”, N=27). Between 9/1/20 and 7/20/21, participants completed a validated CGA (“CGA cohort”, N=67). The results were shared with patients during visits with their BCMC providers. All patients completed a follow-up survey including the Decisional Conflict Scale (DCS). Three providers per clinic from Uro-Oncology, Medical Oncology, and Radiation Oncology also completed the DCS. Time to complete the CGA, completion rates, and patient-reported burden were assessed. Concordance of patient- and provider-reported decisional conflict was compared between Routine and CGA cohorts.
Results: Of 138 eligible patients, 94 patients were successfully enrolled (68%) with median age of 72 years, of whom 18% were women, ECOG PS = 3 in 13%, and Charlson Comorbidity Index = 3 in 18%. Most patients had pT2 bladder cancer (87%; cN+ and M1 in 23.4% and 9.6%, respectively). CGA component completion rates ranged from 79% to 100% (Table). Survey response rates were high (77% for patients, 86% for providers), and most (86%) patients felt that the CGA was at most minimally burdensome. Vulnerabilities detected across CGA domains triggered relevant referrals. Patient-reported median (IQR) DCS scores were numerically higher (greater decisional conflict) for the CGA cohort: (27 [14-33] vs 16 [2-30] for Routine patients, p=0.28). Provider-reported DCS was significantly correlated with patient-reported DCS in the CGA (p=0.04), but not the Routine cohort (p=0.07).
Conclusions: We observed that CGAs were successfully conducted in our BCMC with high rates of completion and low rates of perceived burden but CGA use was not associated with DCS scores. Future work will evaluate associations between individual instruments, clinical outcomes and health-related quality of life.
Source of Funding: Bladder Cancer Advocacy Network Young Investigator Award
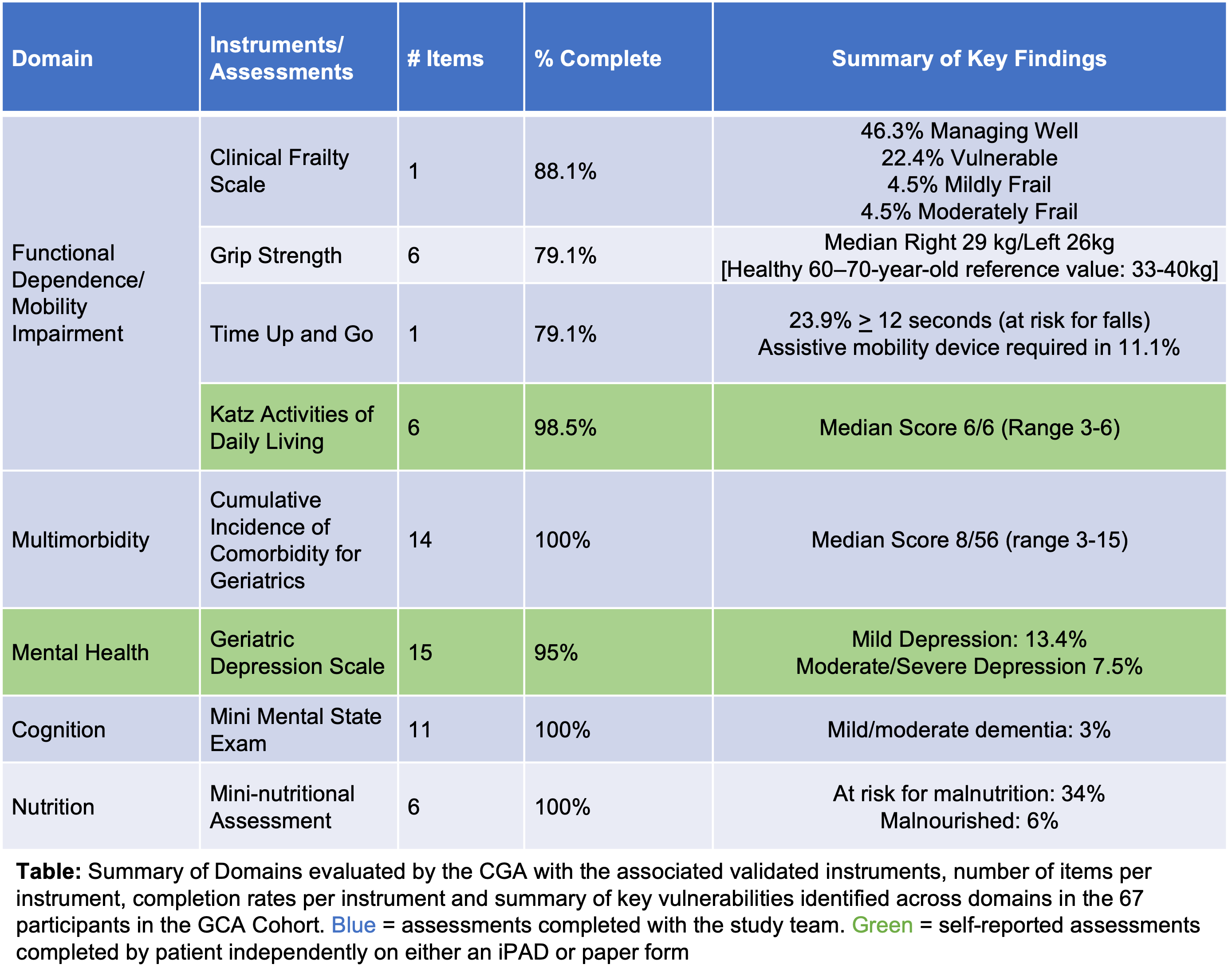
Methods: Patients seen in BCMC were prospectively enrolled from 6/1/20 to 7/20/21. In the first 3 months, participants underwent routine risk stratification (“Routine cohort”, N=27). Between 9/1/20 and 7/20/21, participants completed a validated CGA (“CGA cohort”, N=67). The results were shared with patients during visits with their BCMC providers. All patients completed a follow-up survey including the Decisional Conflict Scale (DCS). Three providers per clinic from Uro-Oncology, Medical Oncology, and Radiation Oncology also completed the DCS. Time to complete the CGA, completion rates, and patient-reported burden were assessed. Concordance of patient- and provider-reported decisional conflict was compared between Routine and CGA cohorts.
Results: Of 138 eligible patients, 94 patients were successfully enrolled (68%) with median age of 72 years, of whom 18% were women, ECOG PS = 3 in 13%, and Charlson Comorbidity Index = 3 in 18%. Most patients had pT2 bladder cancer (87%; cN+ and M1 in 23.4% and 9.6%, respectively). CGA component completion rates ranged from 79% to 100% (Table). Survey response rates were high (77% for patients, 86% for providers), and most (86%) patients felt that the CGA was at most minimally burdensome. Vulnerabilities detected across CGA domains triggered relevant referrals. Patient-reported median (IQR) DCS scores were numerically higher (greater decisional conflict) for the CGA cohort: (27 [14-33] vs 16 [2-30] for Routine patients, p=0.28). Provider-reported DCS was significantly correlated with patient-reported DCS in the CGA (p=0.04), but not the Routine cohort (p=0.07).
Conclusions: We observed that CGAs were successfully conducted in our BCMC with high rates of completion and low rates of perceived burden but CGA use was not associated with DCS scores. Future work will evaluate associations between individual instruments, clinical outcomes and health-related quality of life.
Source of Funding: Bladder Cancer Advocacy Network Young Investigator Award

.jpg)
.jpg)