Back
Poster, Podium & Video Sessions
Podium
PD15: Kidney Cancer: Epidemiology & Evaluation/Staging/Surveillance I
PD15-09: Updated outcomes for active surveillance recommended to all small renal mass patients lacking progression criteria for intervention
Friday, May 13, 2022
4:50 PM – 5:00 PM
Location: Room 245
Muammer Altok, Arun Menon, Ahmed Aly, Tashionna White, James Gaybriella, Bo Xu, Michael Petroziello, Charles Roche, Eric Kauffman*, Buffalo, NY
.jpg)
Eric Curtis Kauffman, MD
Roswell Park Comprehensive Cancer Center
Podium Presenter(s)
Introduction: Despite the indolence of small renal masses (SRM) and lack of known adversity from treatment delays, active surveillance (AS) as a means to risk-stratify SRM patients for more selective treatment is still not widely performed. Here we report updated outcomes for a novel clinical approach in which AS was recommended regardless of health to all SRM patients lacking predefined progression criteria for intervention (PCI).
Methods: All non-end stage renal disease (ESRD) patients with a non-hereditary localized SRM presenting from January 2013 to March 2019 to a single urologic oncologist at a National Comprehensive Cancer Network institute were recommended AS if predefined PCI were absent. Delayed intervention (DI) was recommended only upon PCI development during AS. PCI was defined prospectively as any SRM-related symptoms, unfavorable biopsy histology, cT3a stage, or either of the following in the absence of benign neoplastic biopsy histology: longest tumor diameter (LTD) >4 cm; growth rate >5 mm/year for LTD =3 cm or >3 mm/year for LTD >3 cm. Retrospective review of all SRM patients seen over this 6.25 year period was performed to determine rates of freedom from PCI and DI during AS.
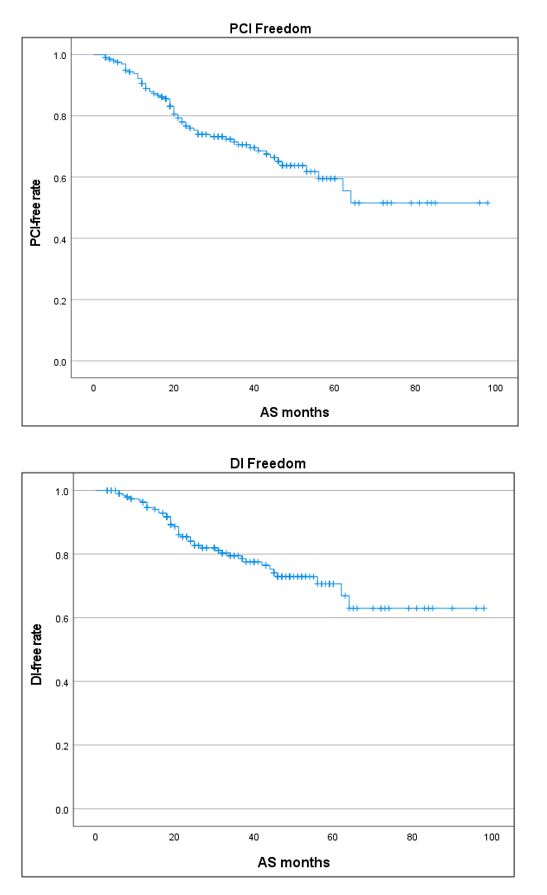
Results: Of 208 total non-ESRD, non-hereditary SRM patients without a prior kidney cancer history, 7 met PCI at presentation. All remaining 201 SRM patients (226 tumors, median LTD 2.2) were managed with AS. With median follow up of 40 months, 59/201 (29%) AS patients developed PCI, of whom 42 (71%) underwent DI (37 resection, 5 ablation). Only 1 (1%) AS patient crossed over to DI without PCI development. 3- and 5-year PCI-free survival rates were 71% and 60%, respectively, and 3- and 5-year DI-free survival rates were 80% and 71%, respectively. Lower PCI-free and DI-free rates were associated with initial LTD and clear cell RCC biopsy histology. DI resections were enriched for pT3 and/or nuclear grade 3-4 malignant pathology, with no benign resections. No AS or DI patient developed metastasis.
Conclusions: AS using predefined PCI in otherwise unselected SRM patients allows intervention to be focused on at-risk SRM cases with common adverse pathology, avoiding treatment for most patients with small renal masses. Long-term DI rates and oncologic safety require further study.
Source of Funding: None
Methods: All non-end stage renal disease (ESRD) patients with a non-hereditary localized SRM presenting from January 2013 to March 2019 to a single urologic oncologist at a National Comprehensive Cancer Network institute were recommended AS if predefined PCI were absent. Delayed intervention (DI) was recommended only upon PCI development during AS. PCI was defined prospectively as any SRM-related symptoms, unfavorable biopsy histology, cT3a stage, or either of the following in the absence of benign neoplastic biopsy histology: longest tumor diameter (LTD) >4 cm; growth rate >5 mm/year for LTD =3 cm or >3 mm/year for LTD >3 cm. Retrospective review of all SRM patients seen over this 6.25 year period was performed to determine rates of freedom from PCI and DI during AS.
Results: Of 208 total non-ESRD, non-hereditary SRM patients without a prior kidney cancer history, 7 met PCI at presentation. All remaining 201 SRM patients (226 tumors, median LTD 2.2) were managed with AS. With median follow up of 40 months, 59/201 (29%) AS patients developed PCI, of whom 42 (71%) underwent DI (37 resection, 5 ablation). Only 1 (1%) AS patient crossed over to DI without PCI development. 3- and 5-year PCI-free survival rates were 71% and 60%, respectively, and 3- and 5-year DI-free survival rates were 80% and 71%, respectively. Lower PCI-free and DI-free rates were associated with initial LTD and clear cell RCC biopsy histology. DI resections were enriched for pT3 and/or nuclear grade 3-4 malignant pathology, with no benign resections. No AS or DI patient developed metastasis.
Conclusions: AS using predefined PCI in otherwise unselected SRM patients allows intervention to be focused on at-risk SRM cases with common adverse pathology, avoiding treatment for most patients with small renal masses. Long-term DI rates and oncologic safety require further study.
Source of Funding: None

.jpg)
.jpg)