Back
Poster, Podium & Video Sessions
Podium
PD15: Kidney Cancer: Epidemiology & Evaluation/Staging/Surveillance I
PD15-12: Impact of the Affordable Care Act on Socioeconomic Disparities in Diagnosis and Survival of Renal Cell Carcinoma
Friday, May 13, 2022
5:20 PM – 5:30 PM
Location: Room 245
Chih Peng Chin*, Micah Levy, Evan Garden, Krishna Ravivarapu, Joseph Sewell Araya, New York, NY, Alexander Small, Bronx, NY, Michael Palese, New York, NY
- CC
Podium Presenter(s)
Introduction: In 2014, the Affordable Care Act (ACA) expanded Medicaid coverage in select states. Our study assesses the impact of ACA expansion on socioeconomic disparities in renal cell carcinoma (RCC) diagnosis and survival.
Methods: Data were obtained from the Surveillance, Epidemiology, and End Results (SEER) database from 2010-2013 (pre-ACA) and 2015-2018 (post-ACA) in states with ACA expansion (CA, CT, HI, IA, KY, NJ, NM, WA) or without ACA expansion (GA, UT). Socioeconomic factors (SEF) included insurance status, county-level median family income and % persons >25-years-old with =high school education. Quintiles were calculated for county-level SEFs, and outcomes between the 1st and 5th quintiles were compared. Disparity was measured as the difference in malignancy outcomes (diagnosis stage and 2-year survival) between patients in the 1st and 5th quintile of county-level SEFs.
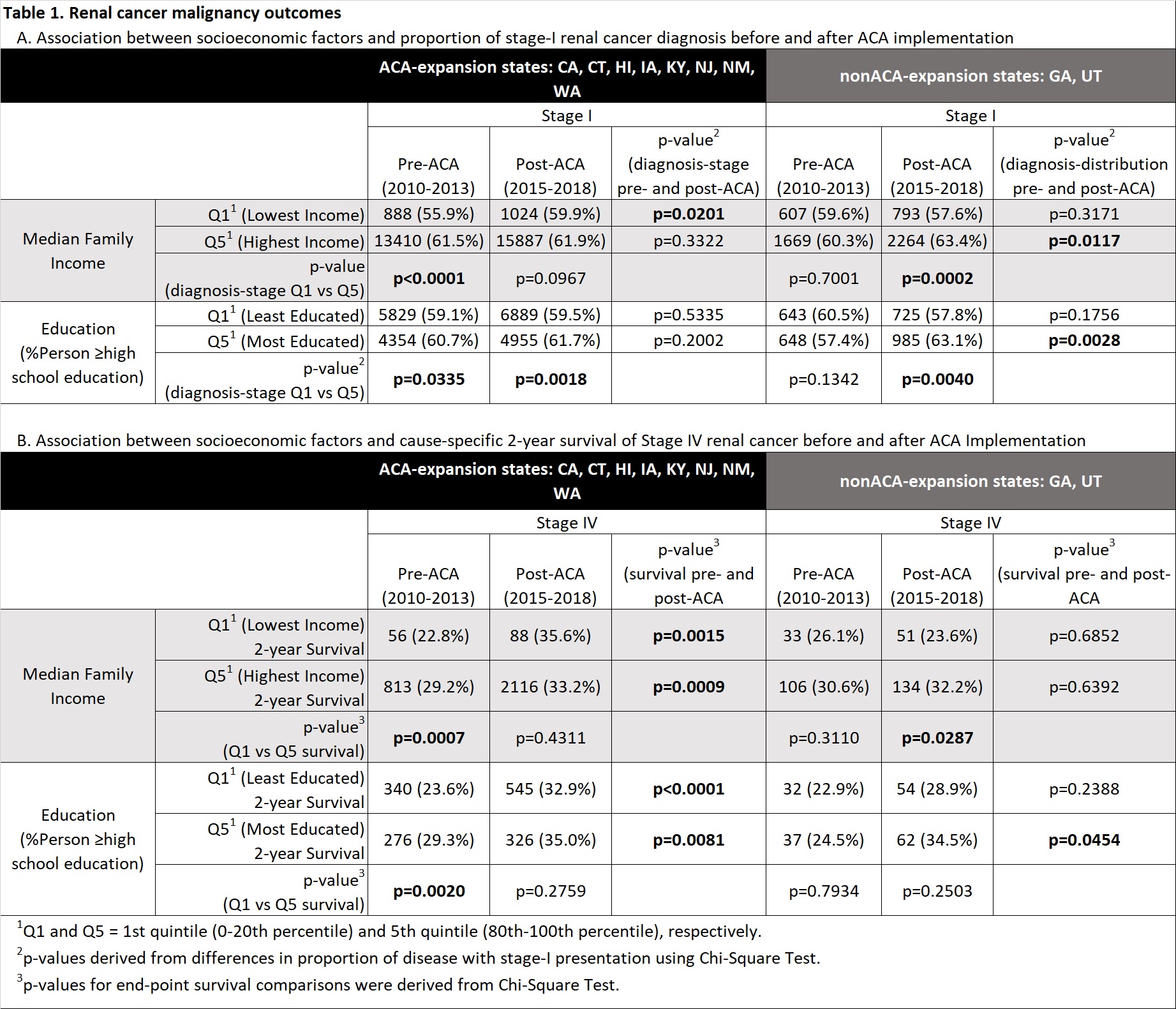
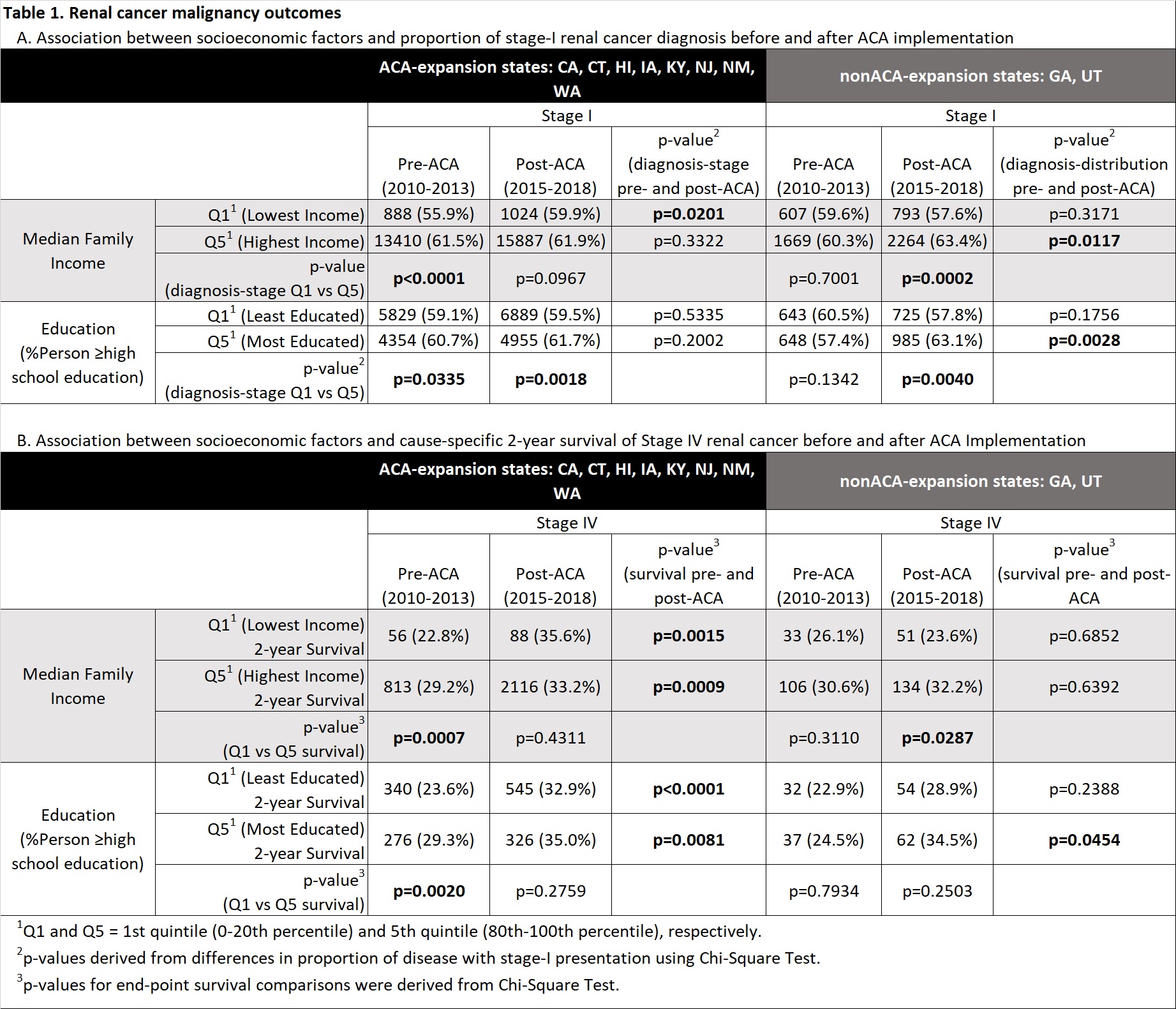
Results: Results are summarized in Table 1. We identified 100,122 cases of RCC including 84,617 (85%) in ACA expansion and 15,505 (15%) in non-ACA-expansion states. Post-ACA, uninsured patients diagnosed with RCC decreased in expansion states (2.8% to 1.2%, p<0.01) but not in non-expansion states (5.0% to 4.4%, p=0.07). In expansion states pre-ACA, high-income patients were more likely to present with stage I (61.5% vs 55.9%, p<0.01) and less likely to present with stage IV disease (16.5% vs 18.8%, p<0.01). Post-ACA, the association between income disparity and disease stage diminished (stage I 59.9% vs 61.9%, p=0.10 and stage IV 17.3% vs 15.8%, p=0.10). On the contrary, in non-expansion states, significant income and education disparities in diagnosis-stage were not observed pre-ACA but developed post-ACA. Regarding education-level, diagnosis stage remained consistent in expansion states pre- and post-ACA. Advanced disease survival differed significantly by SEF. In expansion-states, pre-ACA patients in high-income and more educated counties had greater 2-year survival for stage III and IV disease. This difference became statistically insignificant post-ACA. In non-expansion states, SEF disparities did not result in significant survival differences pre- or post-ACA.
Conclusions: ACA expansion was associated with significantly decreased top-to-bottom SEF disparities in RCC diagnosis and advanced RCC survival.
Source of Funding: None
Methods: Data were obtained from the Surveillance, Epidemiology, and End Results (SEER) database from 2010-2013 (pre-ACA) and 2015-2018 (post-ACA) in states with ACA expansion (CA, CT, HI, IA, KY, NJ, NM, WA) or without ACA expansion (GA, UT). Socioeconomic factors (SEF) included insurance status, county-level median family income and % persons >25-years-old with =high school education. Quintiles were calculated for county-level SEFs, and outcomes between the 1st and 5th quintiles were compared. Disparity was measured as the difference in malignancy outcomes (diagnosis stage and 2-year survival) between patients in the 1st and 5th quintile of county-level SEFs.
Results: Results are summarized in Table 1. We identified 100,122 cases of RCC including 84,617 (85%) in ACA expansion and 15,505 (15%) in non-ACA-expansion states. Post-ACA, uninsured patients diagnosed with RCC decreased in expansion states (2.8% to 1.2%, p<0.01) but not in non-expansion states (5.0% to 4.4%, p=0.07). In expansion states pre-ACA, high-income patients were more likely to present with stage I (61.5% vs 55.9%, p<0.01) and less likely to present with stage IV disease (16.5% vs 18.8%, p<0.01). Post-ACA, the association between income disparity and disease stage diminished (stage I 59.9% vs 61.9%, p=0.10 and stage IV 17.3% vs 15.8%, p=0.10). On the contrary, in non-expansion states, significant income and education disparities in diagnosis-stage were not observed pre-ACA but developed post-ACA. Regarding education-level, diagnosis stage remained consistent in expansion states pre- and post-ACA. Advanced disease survival differed significantly by SEF. In expansion-states, pre-ACA patients in high-income and more educated counties had greater 2-year survival for stage III and IV disease. This difference became statistically insignificant post-ACA. In non-expansion states, SEF disparities did not result in significant survival differences pre- or post-ACA.
Conclusions: ACA expansion was associated with significantly decreased top-to-bottom SEF disparities in RCC diagnosis and advanced RCC survival.
Source of Funding: None

.jpg)
.jpg)