Back
Poster, Podium & Video Sessions
Podium
PD17: Prostate Cancer: Detection & Screening III
PD17-05: Characteristics and outcomes of patients with PIRADS 5 lesions and negative biopsies
Saturday, May 14, 2022
7:40 AM – 7:50 AM
Location: Room 252
Eric Li*, Mohammad Siddiqui, Jonathan Aguiar, Brandon Ansbro, Parth Shah, Moataz Soliman, Jordan Rich, Jasmine Lin, Johan Alfaro Carballo, Mary Kate Keeter, Quan Mai, Edward Schaeffer, Ashley Ross, Chicago, IL
- EL
Podium Presenter(s)
Introduction: Best evidence supports use of mpMRI prior to initial diagnosis of prostate cancer. PIRADS 5 lesions typically have a 80-90% concordance with diagnosis of clinically significant disease. Here we investigate the characteristics and outcomes of patients with PIRADS 5 lesions and subsequent negative biopsies.
Methods: We queried our institutional database for men without an established diagnosis of prostate cancer for whom MRI targeted biopsy was performed after demonstration of a PIRADS 5 lesion from March 2018-present. T test, chi-squared test, and logistic regression were performed.
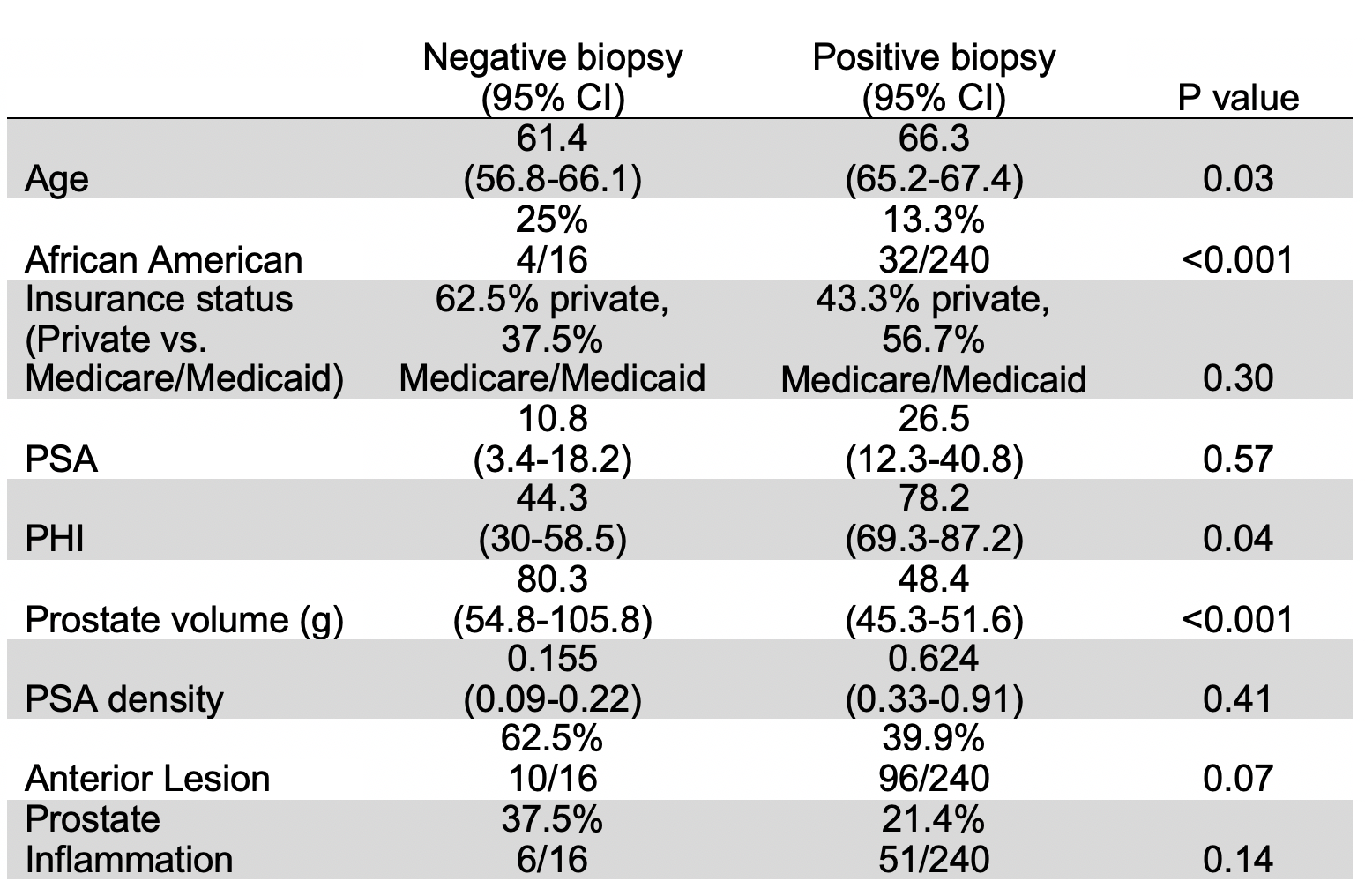
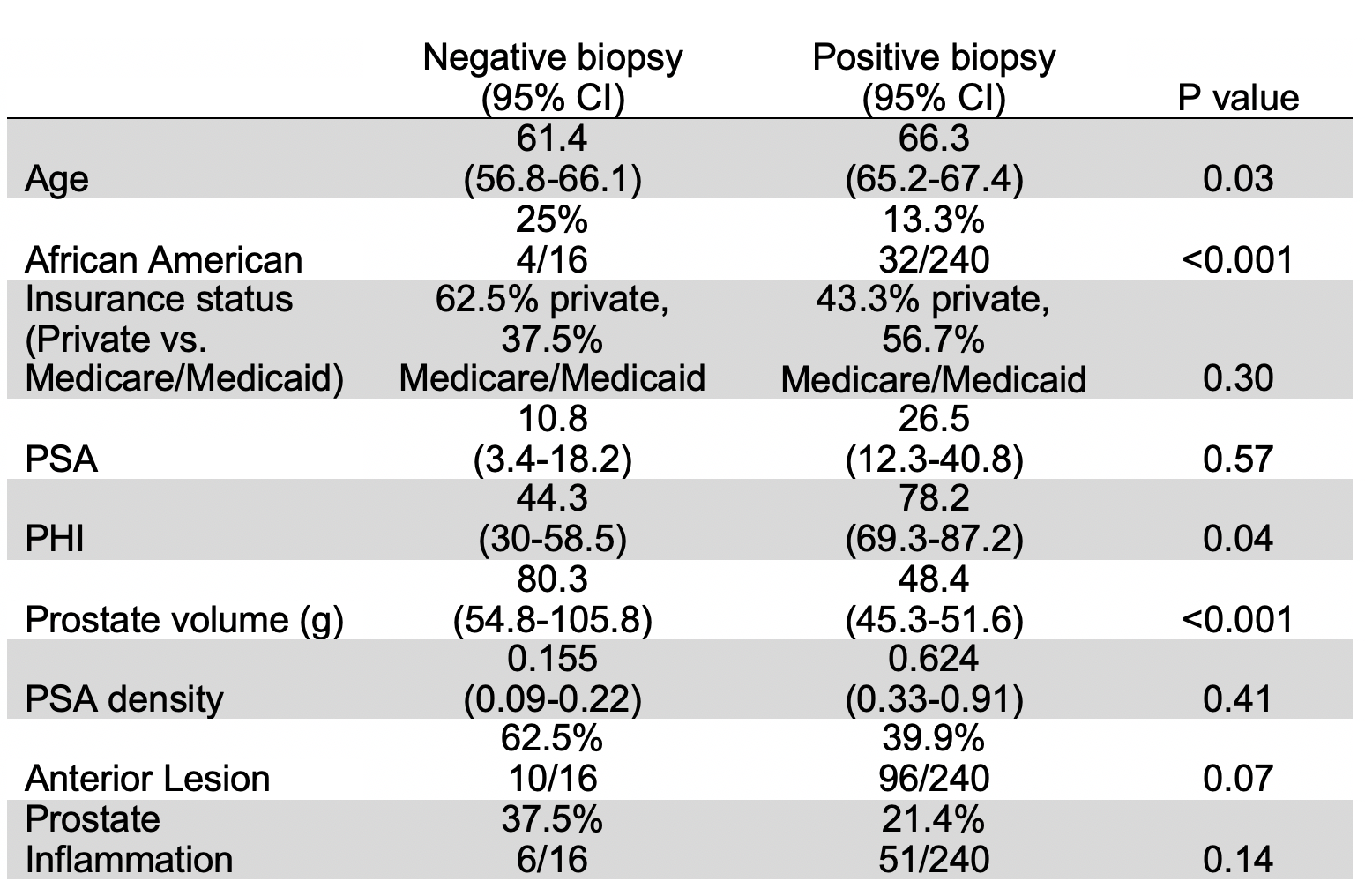
Results: 2,206 men underwent MRI for suspicion of prostate cancer, with PIRADS 5 lesions detected in 268 patients. 257 of these men underwent prostate biopsy (13 with transperineal biopsy) with a positivity rate of 93.8%. Men with PIRADS 5 lesions and negative biopsies (n=16) were more likely to be African American (25% vs 13.3%, p<0.001), younger (61.4 vs 66.3, p=0.03), have larger prostates (80.3 g vs 48.4 g, p<0.001), and have lower prostate health index (PHI, 44.3 vs. 78.2, p=0.04). There was no significant difference in anterior lesions, prostate inflammation, PSA, or PSA density. Of men with negative prostate biopsies, 1 patient was subsequently diagnosed with prostate cancer, and 2 patients had bladder outlet procedures with negative pathology. 2 patients with negative biopsies previously received BCG for non-muscle invasive bladder cancer and were subsequently found to have inflammation on prostate biopsy.
Conclusions: Men with PIRADS 5 lesions and negative prostate biopsies tend to be African American, younger, have larger prostates, and have lower PHI compared to patients with positive prostate biopsies. Additional investigation is needed to determine lesion location is a risk factor for undersampling that may benefit from transperineal prostate biopsy, as well as the role of inflammation in determining how to follow these patients.
Source of Funding: None
Methods: We queried our institutional database for men without an established diagnosis of prostate cancer for whom MRI targeted biopsy was performed after demonstration of a PIRADS 5 lesion from March 2018-present. T test, chi-squared test, and logistic regression were performed.
Results: 2,206 men underwent MRI for suspicion of prostate cancer, with PIRADS 5 lesions detected in 268 patients. 257 of these men underwent prostate biopsy (13 with transperineal biopsy) with a positivity rate of 93.8%. Men with PIRADS 5 lesions and negative biopsies (n=16) were more likely to be African American (25% vs 13.3%, p<0.001), younger (61.4 vs 66.3, p=0.03), have larger prostates (80.3 g vs 48.4 g, p<0.001), and have lower prostate health index (PHI, 44.3 vs. 78.2, p=0.04). There was no significant difference in anterior lesions, prostate inflammation, PSA, or PSA density. Of men with negative prostate biopsies, 1 patient was subsequently diagnosed with prostate cancer, and 2 patients had bladder outlet procedures with negative pathology. 2 patients with negative biopsies previously received BCG for non-muscle invasive bladder cancer and were subsequently found to have inflammation on prostate biopsy.
Conclusions: Men with PIRADS 5 lesions and negative prostate biopsies tend to be African American, younger, have larger prostates, and have lower PHI compared to patients with positive prostate biopsies. Additional investigation is needed to determine lesion location is a risk factor for undersampling that may benefit from transperineal prostate biopsy, as well as the role of inflammation in determining how to follow these patients.
Source of Funding: None

.jpg)
.jpg)