Back
Poster, Podium & Video Sessions
Podium
PD17: Prostate Cancer: Detection & Screening III
PD17-06: Active Surveillance Discontinuation Among Low-Risk Prostate Cancer Patients: Results from a Large National Database
Saturday, May 14, 2022
7:50 AM – 8:00 AM
Location: Room 252
Rashid Sayyid*, Augusta, GA, Laurence Klotz, Toronto, Canada, John Benton, Martha Terris, Augusta, GA, Christopher Wallis, Toronto, Canada, Zachary Klaassen, Augusta, GA

Rashid Sayyid, MD
Augusta University
Podium Presenter(s)
Introduction: A substantial proportion of prostate cancer (PCa) patients on active surveillance (AS) undergo definitive treatment within ten years of diagnosis. Patient factors influencing decision to opt for definitive therapy, and, specifically, choice of radical prostatectomy (RP) versus radiation therapy (XRT) remain unclear.
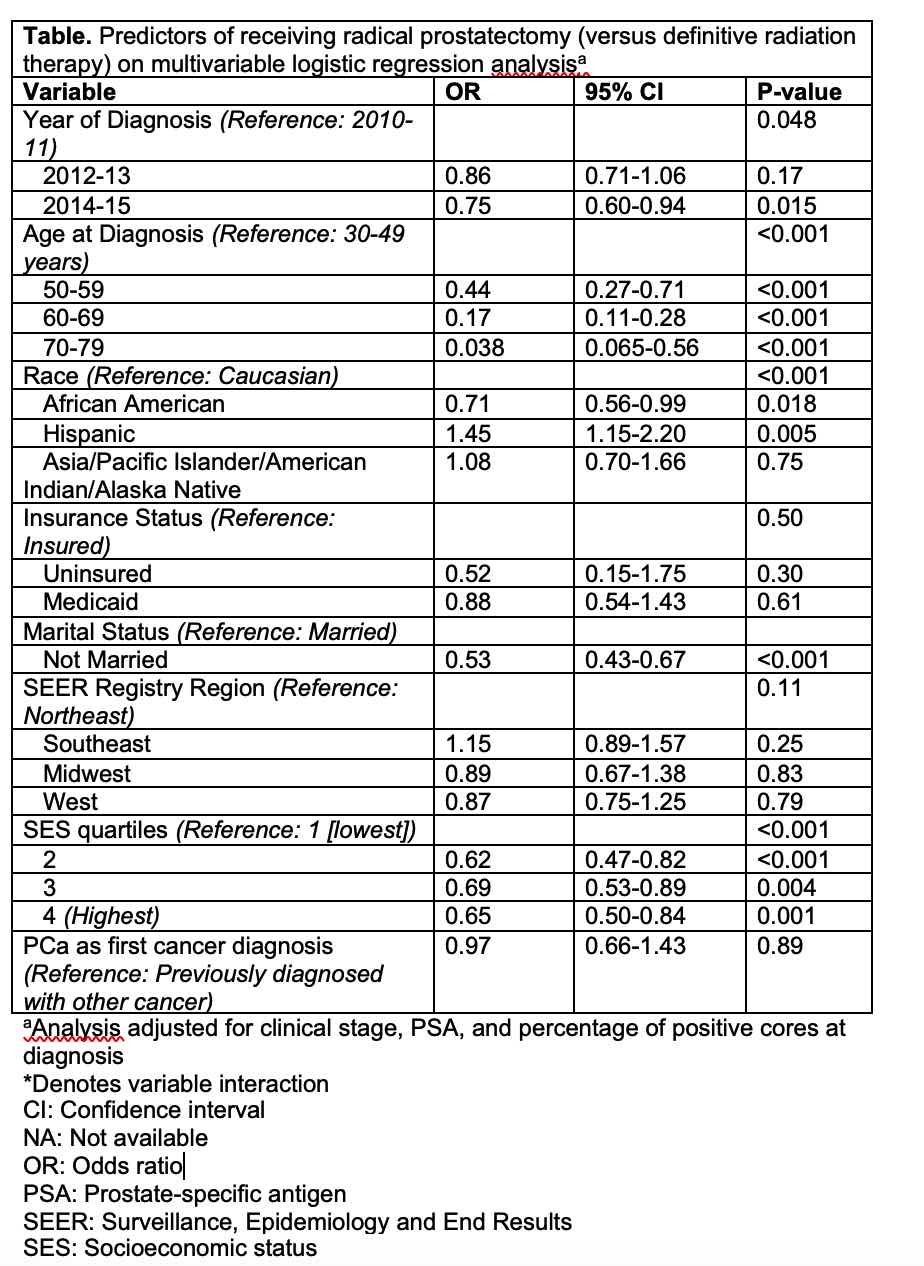
Methods: The Surveillance, Epidemiology, and End Results (SEER) Prostate with Watchful Waiting database was used to identify patients diagnosed with NCCN low-risk PCa between 2010 and 2015, managed with AS for at least one year following diagnosis. We sought to determine sociodemographic and oncologic predictors both of undergoing definitive intervention regardless of modality and of RP versus XRT, using multivariable logistic regression analysis.
Results: The study cohort included 32,874 men. 21,255 (64.7%) patients underwent delayed treatment, with 3,751 (17.6%) and 17,463 (82.4%) opting for RP and XRT, respectively. Median patient age was 64.0 years, 5,353 (16.3%) were African-American, and median PSA was 5.3 ng/ml.
In addition to higher clinical stage, PSA at diagnosis and percent core involvement, multiple sociodemographic factors were associated with increased odds of receiving intervention on multivariable analysis: older age at diagnosis (odds ratio [OR] 1.33, p=0.007), diagnosis in the Southeast (OR 1.26, p <0.001) or Midwest (OR 1.22, p=0.021), and higher socioeconomic status (SES) (OR 1.67, p<0.001). Men who were uninsured (OR 0.34, p <0.001), had Medicaid (OR 0.82, p=0.024), or were not married (OR 0.85, p <0.001) were less likely to undergo definitive treatment.
Sociodemographic factors predicting decreased odds of choosing RP (i.e. higher odds of receiving XRT) amongst patients opting for delayed treatment included: older age at diagnosis (OR 0.038,p < 0.001), African American race (OR 0.71, p=0.018), unmarried status (OR 0.53, p<0.001), and higher SES (highest vs. lowest OR 0.65, p=0.001).
Conclusions: The majority of low-risk PCa patients initially managed with AS underwent delayed treatment, with decision for discontinuation of AS and choice of RP versus XRT, in those who opt for definitive intervention, significantly associated with multiple sociodemographic and oncologic variables.
Source of Funding: None
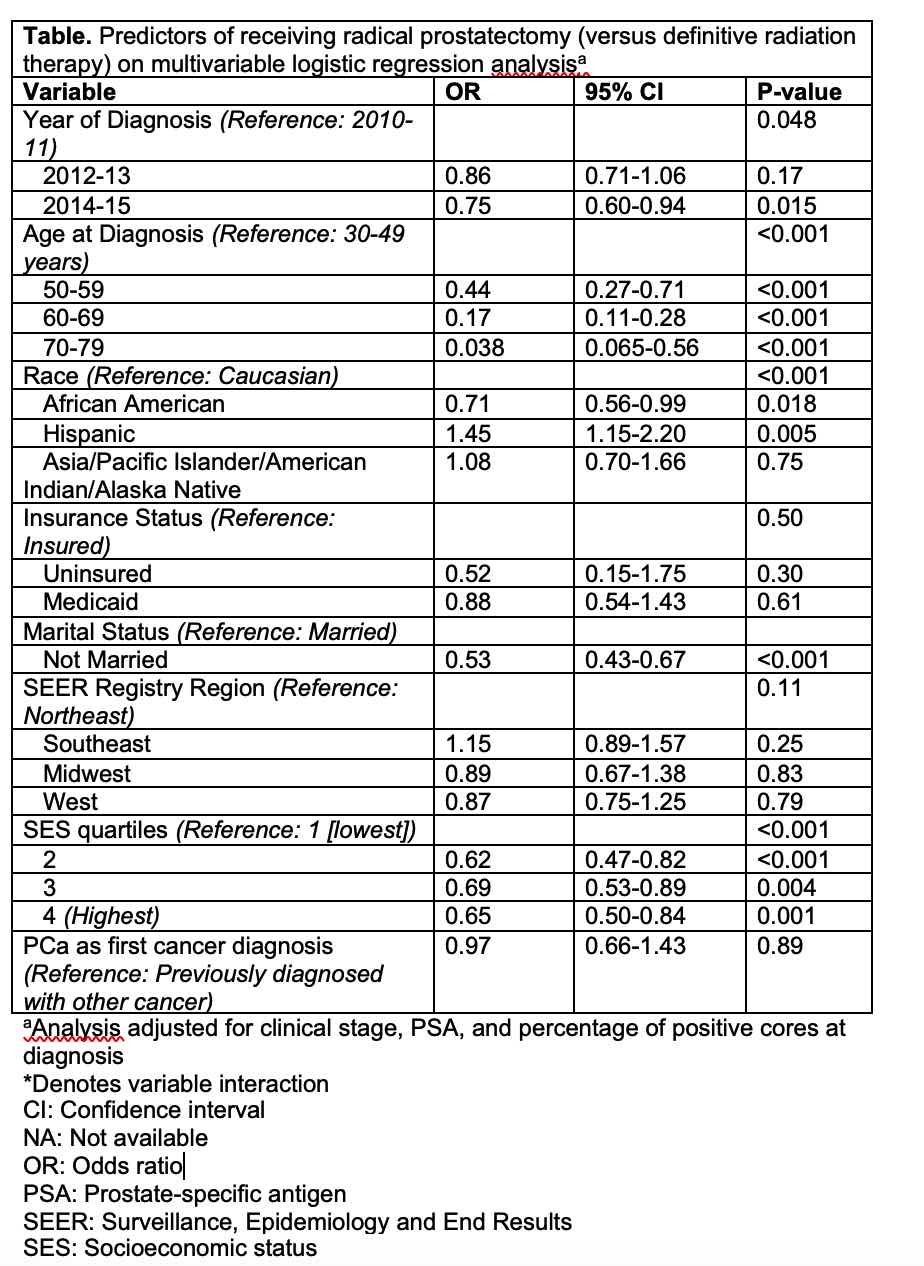
Methods: The Surveillance, Epidemiology, and End Results (SEER) Prostate with Watchful Waiting database was used to identify patients diagnosed with NCCN low-risk PCa between 2010 and 2015, managed with AS for at least one year following diagnosis. We sought to determine sociodemographic and oncologic predictors both of undergoing definitive intervention regardless of modality and of RP versus XRT, using multivariable logistic regression analysis.
Results: The study cohort included 32,874 men. 21,255 (64.7%) patients underwent delayed treatment, with 3,751 (17.6%) and 17,463 (82.4%) opting for RP and XRT, respectively. Median patient age was 64.0 years, 5,353 (16.3%) were African-American, and median PSA was 5.3 ng/ml.
In addition to higher clinical stage, PSA at diagnosis and percent core involvement, multiple sociodemographic factors were associated with increased odds of receiving intervention on multivariable analysis: older age at diagnosis (odds ratio [OR] 1.33, p=0.007), diagnosis in the Southeast (OR 1.26, p <0.001) or Midwest (OR 1.22, p=0.021), and higher socioeconomic status (SES) (OR 1.67, p<0.001). Men who were uninsured (OR 0.34, p <0.001), had Medicaid (OR 0.82, p=0.024), or were not married (OR 0.85, p <0.001) were less likely to undergo definitive treatment.
Sociodemographic factors predicting decreased odds of choosing RP (i.e. higher odds of receiving XRT) amongst patients opting for delayed treatment included: older age at diagnosis (OR 0.038,p < 0.001), African American race (OR 0.71, p=0.018), unmarried status (OR 0.53, p<0.001), and higher SES (highest vs. lowest OR 0.65, p=0.001).
Conclusions: The majority of low-risk PCa patients initially managed with AS underwent delayed treatment, with decision for discontinuation of AS and choice of RP versus XRT, in those who opt for definitive intervention, significantly associated with multiple sociodemographic and oncologic variables.
Source of Funding: None

.jpg)
.jpg)