Back
Poster, Podium & Video Sessions
Podium
PD17: Prostate Cancer: Detection & Screening III
PD17-07: PSA Testing and Colorectal Cancer Screening Trends from 2012 to 2020: Analysis of the CDC Behavioral Risk Factor Surveillance System (BRFSS)
Saturday, May 14, 2022
8:00 AM – 8:10 AM
Location: Room 252
Anh Nguyen*, John Fastenau, Gabriel Fernandez, Courtney Berg, Amjad Alwaal, Evan Kovac, Robert Weiss, Newark, NJ

Anh T. Nguyen, MD
Rutgers NJMS
Podium Presenter(s)
Introduction: In 2021 it is estimated that there will be 248,530 new cases of prostate cancer with 34,130 deaths, and 149,500 new cases of colorectal cases with 52,900 deaths. Before 2012, prostate specific antigen (PSA) screening was performed at a higher rate than colorectal cancer (CRC). The USPTF recommends colorectal screen for adults between the ages of 50-75, while it recommends shared decision-making regarding PSA testing for men between the ages of 55-69. We sought to compare PSA screening to CRC screening from 2012-2020. Data was stratified by income, geographic region, race and health insurance.
Methods: We used the CDC’s BRFSS, a national database of surveys on health-related behaviors and preventive medical services. We examined bi-yearly data on PSA testing for men aged 50+ and corresponding CRC screening data (colonoscopy and sigmoidoscopy). Income, geographic region, self-identified race, and health insurance status were examined.
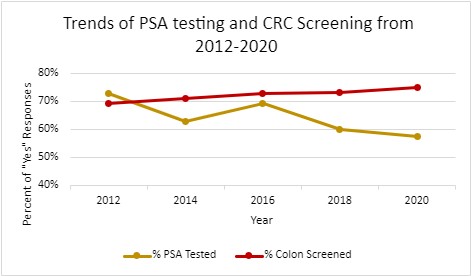
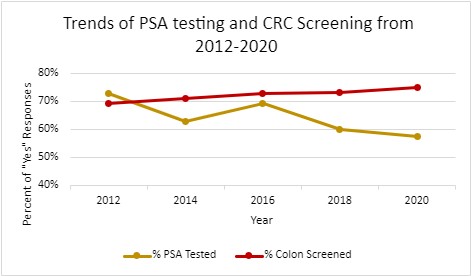
Results: 367,535 men, aged 50+ responded if they had PSA testing and CRC screening and answered demographic questions from 2012-2020. PSA testing decreased from 73.0% of respondents in 2012 to 57.7% in 2020. CRC screening increased from 69.5% in 2012 to 75.1% in 2020.
CRC screening was the most influential on adherence to PSA testing [OR] = 4.69. Having health insurance was a positive predictor of PSA adherence [OR] = 2.73 and CRC [OR] = 3.18. Those with lower income were less likely to receive PSA testing [OR] = 0.36 and CRC screening [OR] = 0.31. PSA testing increased with age until 80 years and CRC screening increased until 75 years then both decreased. The Mid-Atlantic region had the highest adherence to PSA testing, whereas the North East region had the highest CRC screening. Non-Hispanic White and non-Hispanic Black men were most likely to have received a PSA test compared to other racial groups.
Conclusions: PSA testing among men age 50+ has decreased from 2012 to 2020 while CRC screening has increased which reflects respective USPTF guidance. Men who underwent CRC screening were four times more likely to get PSA testing. Decreasing rates of PSA testing has implications in detection and severity of prostate cancer on diagnosis. Observed trends among lower income levels, minority groups, and uninsured men demonstrate disparities in PSA testing.
Source of Funding: None
Methods: We used the CDC’s BRFSS, a national database of surveys on health-related behaviors and preventive medical services. We examined bi-yearly data on PSA testing for men aged 50+ and corresponding CRC screening data (colonoscopy and sigmoidoscopy). Income, geographic region, self-identified race, and health insurance status were examined.
Results: 367,535 men, aged 50+ responded if they had PSA testing and CRC screening and answered demographic questions from 2012-2020. PSA testing decreased from 73.0% of respondents in 2012 to 57.7% in 2020. CRC screening increased from 69.5% in 2012 to 75.1% in 2020.
CRC screening was the most influential on adherence to PSA testing [OR] = 4.69. Having health insurance was a positive predictor of PSA adherence [OR] = 2.73 and CRC [OR] = 3.18. Those with lower income were less likely to receive PSA testing [OR] = 0.36 and CRC screening [OR] = 0.31. PSA testing increased with age until 80 years and CRC screening increased until 75 years then both decreased. The Mid-Atlantic region had the highest adherence to PSA testing, whereas the North East region had the highest CRC screening. Non-Hispanic White and non-Hispanic Black men were most likely to have received a PSA test compared to other racial groups.
Conclusions: PSA testing among men age 50+ has decreased from 2012 to 2020 while CRC screening has increased which reflects respective USPTF guidance. Men who underwent CRC screening were four times more likely to get PSA testing. Decreasing rates of PSA testing has implications in detection and severity of prostate cancer on diagnosis. Observed trends among lower income levels, minority groups, and uninsured men demonstrate disparities in PSA testing.
Source of Funding: None

.jpg)
.jpg)