Back
Poster, Podium & Video Sessions
Podium
PD19: Stone Disease: Surgical Therapy (including ESWL) II
PD19-11: Narcotic Free Ureteroscopic Laser Lithotripsy: A Prospective Randomized Study
Saturday, May 14, 2022
8:40 AM – 8:50 AM
Location: Room 245
Jacob Bamberger*, Brooklyn, NY, Blair Gallante, Anna Zampini, William M Atallah, Johnathan A Khusid, Areeba S Sadiq, Alan Yaghoubian, Mantu Gupta, New York, NY
- JB
Podium Presenter(s)
Introduction: Prescription opioid abuse has reached epidemic levels in the US, fueled in part by unused prescription narcotic reservoirs within communities. The aim of this study is to evaluate the efficacy of non-narcotic analgesics and preoperative counseling in managing post-operative pain following ureteroscopic laser lithotripsy (URS).
Methods: Adult patients at a single academic center undergoing URS for urolithiasis were recruited. Exclusion criteria were: pre-existing stent, contradictions to oxycodone, acetaminophen, or ibuprofen, or current prescription analgesic use. After informed consent, subjects were randomized into 3 groups: 1. Narcotic-only (OXY)—15 oxycodone-acetaminophen 5/325mg, 2. NSAID-only (IBU)—15 ibuprofen 600mg, 3. Counseling (CNSL)—15 oxycodone-acetaminophen 5/325mg, 15 ibuprofen 600mg, and preoperative counseling from the surgeon to avoid narcotic if possible. Patients in whom stent placement was deemed unnecessary intraoperatively were excluded. At the time of stent removal subjects completed the Universal Stent Symptom Questionnaire (USSQ) and a pill count was performed. USSQ pain indices and analgesic consumption were primary and secondary study endpoints, respectively. Demographic, operative, and postoperative data were analyzed between the three groups.
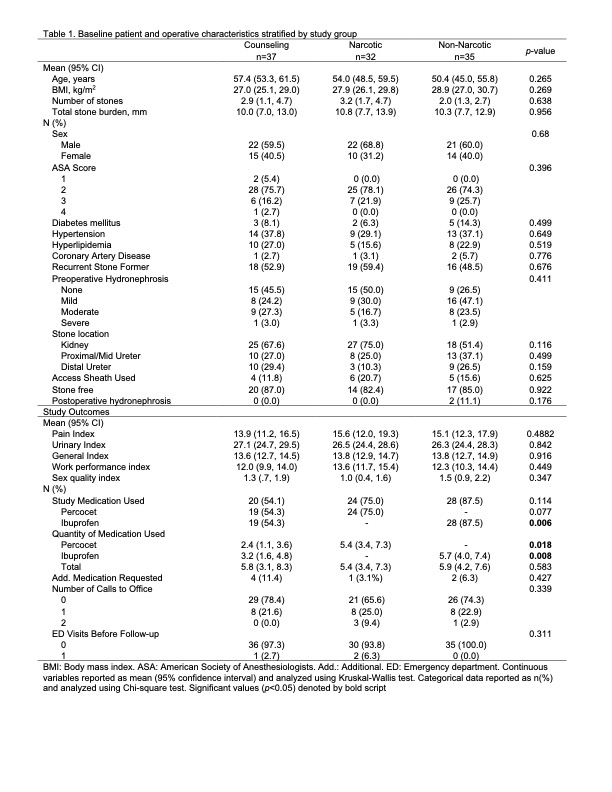
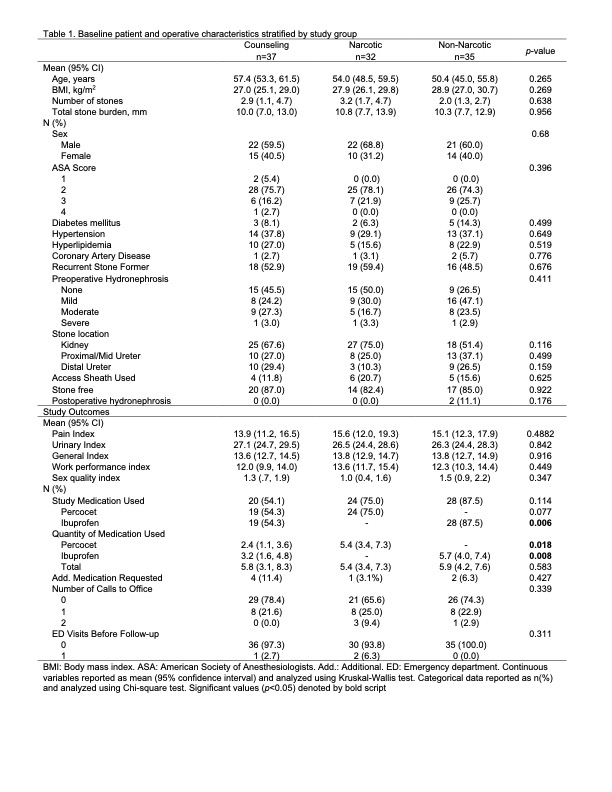
Results: Of 115 patients who completed the study, 104 were eligible for analysis and 11 were lost to follow-up. No significant differences were noted in patient demographic, clinical or operative characteristics. No differences were noted in mean USSQ pain indices across the three groups. The counseling group used a significantly lower number of OXY pills compared to the narcotic group (2.4 vs. 5.4, p=0.018), and less IBU compared to the non-narcotic group (3.2 vs. 5.7, p=0.008), however no differences in mean total pill count were noted between groups (Table 1).
Conclusions: Our data suggest that patients can achieve equivalent post-operative analgesic satisfaction with non-narcotic pain medication compared to opiates following URS. Further, counseling patients on post-operative pain before surgery can reduce the total number of postoperative narcotic and non-narcotic medications taken.We suggest surgeons strongly consider omission of narcotic prescriptions following non-complicated URS.
Source of Funding: N/A
Methods: Adult patients at a single academic center undergoing URS for urolithiasis were recruited. Exclusion criteria were: pre-existing stent, contradictions to oxycodone, acetaminophen, or ibuprofen, or current prescription analgesic use. After informed consent, subjects were randomized into 3 groups: 1. Narcotic-only (OXY)—15 oxycodone-acetaminophen 5/325mg, 2. NSAID-only (IBU)—15 ibuprofen 600mg, 3. Counseling (CNSL)—15 oxycodone-acetaminophen 5/325mg, 15 ibuprofen 600mg, and preoperative counseling from the surgeon to avoid narcotic if possible. Patients in whom stent placement was deemed unnecessary intraoperatively were excluded. At the time of stent removal subjects completed the Universal Stent Symptom Questionnaire (USSQ) and a pill count was performed. USSQ pain indices and analgesic consumption were primary and secondary study endpoints, respectively. Demographic, operative, and postoperative data were analyzed between the three groups.
Results: Of 115 patients who completed the study, 104 were eligible for analysis and 11 were lost to follow-up. No significant differences were noted in patient demographic, clinical or operative characteristics. No differences were noted in mean USSQ pain indices across the three groups. The counseling group used a significantly lower number of OXY pills compared to the narcotic group (2.4 vs. 5.4, p=0.018), and less IBU compared to the non-narcotic group (3.2 vs. 5.7, p=0.008), however no differences in mean total pill count were noted between groups (Table 1).
Conclusions: Our data suggest that patients can achieve equivalent post-operative analgesic satisfaction with non-narcotic pain medication compared to opiates following URS. Further, counseling patients on post-operative pain before surgery can reduce the total number of postoperative narcotic and non-narcotic medications taken.We suggest surgeons strongly consider omission of narcotic prescriptions following non-complicated URS.
Source of Funding: N/A

.jpg)
.jpg)