Back
Poster, Podium & Video Sessions
Podium
PD20: Infertility: Epidemiology & Evaluation II
PD20-04: Does air pollution impact on semen parameters: findings from a real-life cross-sectional study in white-European infertile men
Saturday, May 14, 2022
7:30 AM – 7:40 AM
Location: Room 244
Federico Belladelli*, Giuseppe Fallara, Edoardo Pozzi, Massimiliano Raffo, Christian Corsini, Luigi Candela, Antonio Costa, Daniele Cignoli, Nicolò Schifano, Alessia d'Arma, Milan, Italy, Paolo Capogrosso, Varese, Italy, Luca Boeri, Eugenio Ventimiglia, Rayan Matloob, Luca Pagliardini, Enrico Papaleo, Milan, Italy, Vincenzo Mirone, Naples, Italy, Francesco Montorsi, Andrea Salonia, Milan, Italy
- FB
Podium Presenter(s)
Introduction: Air pollutants levels have been monitored closely for environmental and research issues in industrialized countries. We aimed to investigate the association between air pollutants levels and semen parameters in a cohort of white-European men seeking medical attention for primary couple’s infertility in Italy.
Methods: Complete demographic and laboratory data from 1152 infertile men consecutively assessed between 01/2015 and 12/2019 were analysed. Semen analyses were based on the 2010 WHO reference criteria. Health-significant comorbidities were scored with the Charlson Comorbidity Index (CCI). We analyzed the annual average level of the three main markers of air pollution (Pm10, Pm2.5, and NO2) between 2014-2018 (Legambiente, 2020, Annual dossier series on air quality in Italy, referring the European Environmental Agency) relative to patients’ addresses over the last 5 years. Descriptive statistics and linear regression analyses were used to test the association between air pollutants levels and semen parameters.
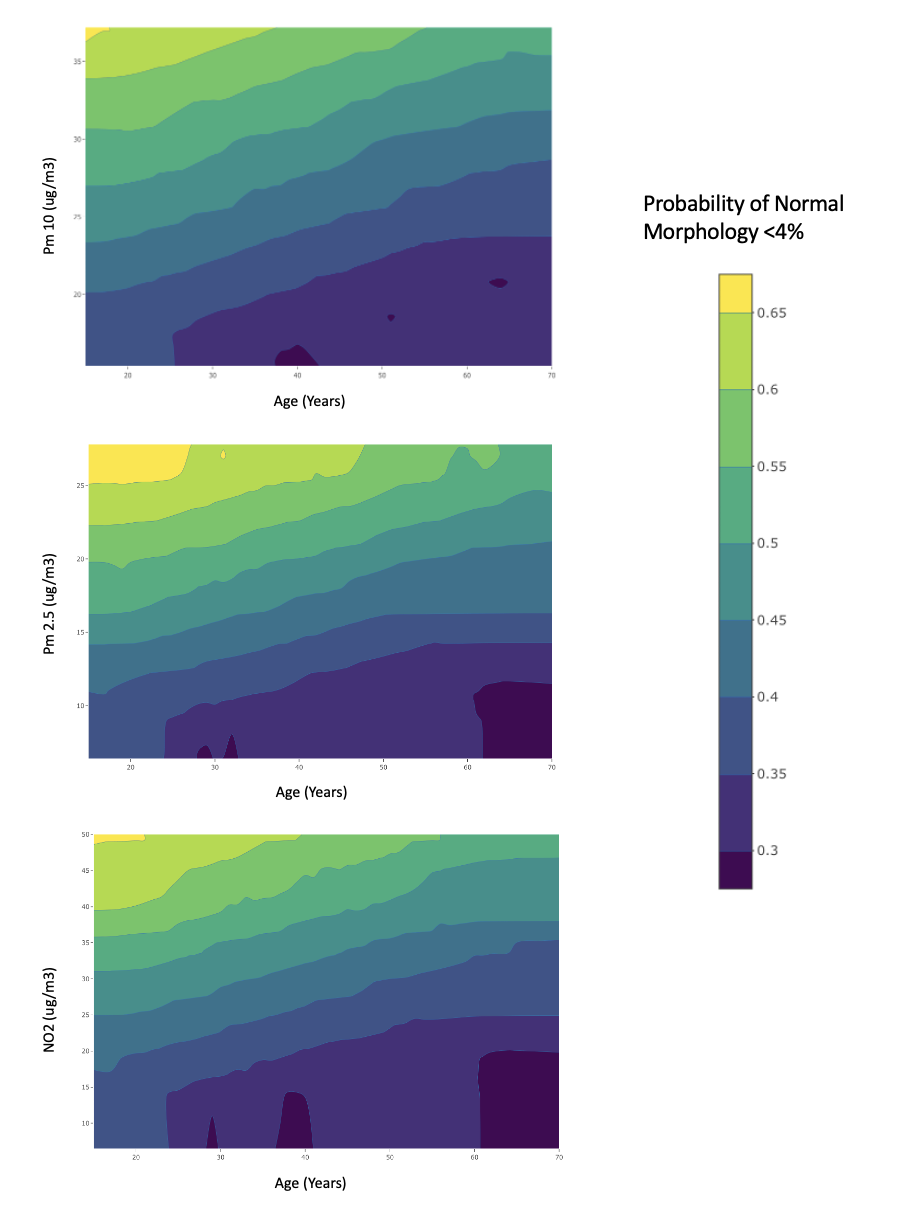
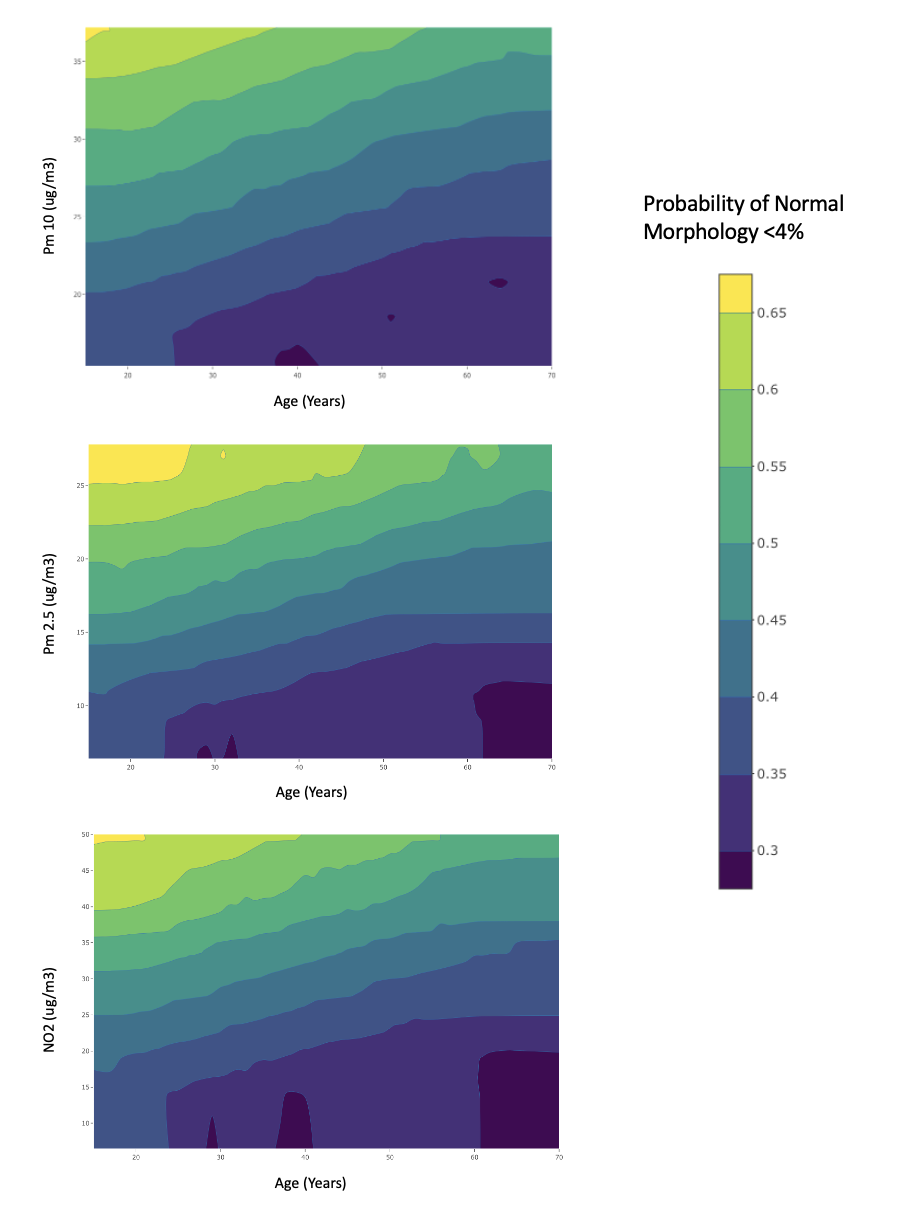
Results: Overall, median (IQR) age and BMI were 37 (33-41) years and 24.3 (22.7-26.5) kg/m2, respectively. A CCI score = 1 was found in 98 (8.5%) men, and 318 (27.6%) participants were active smokers. Of 1152 men, 87 (7.6%) had normal sperm parameters. Of 1065 patients with abnormal semen analyses, 237 (22.3%), 324 (30.4%), and 287 (27.0%) patients presented 1, 2 or 3 abnormalities, respectively; 217 (20.38%) patients were azoospermic. At linear regression analysis, Pm10, Pm2.5, and NO2 were negatively associated with sperm morphology (Pm10: ß: -0.5288 µg/m3, p=0.001; Pm2.5: ß: -0.5240 µg/m3, p=0.019; NO2: ß: -0.4396 µg/m3, p<0.0001). Furthermore, the adjusted odds of sperm normal morphology <4% were 1.06 (95% CI 1.03-1.09; p=0.007) for Pm10, 1.07 (95% CI 1.03-1.11; p=0.007) for Pm 2.5, and 1.03 (95% CI 1.02-1.05; p=0.001) for NO2, respectively (Fig.1).
Conclusions: Findings of this cross-sectional study showed that Pm10, Pm 2.5, and NO2 levels were negatively associated with sperm morphology; conversely, they were not consistently associated with an increased risk of other abnormal sperm parameters in infertile men. Further studies are needed to better characterize air pollution effects on sperm parameters.
Source of Funding: None
Methods: Complete demographic and laboratory data from 1152 infertile men consecutively assessed between 01/2015 and 12/2019 were analysed. Semen analyses were based on the 2010 WHO reference criteria. Health-significant comorbidities were scored with the Charlson Comorbidity Index (CCI). We analyzed the annual average level of the three main markers of air pollution (Pm10, Pm2.5, and NO2) between 2014-2018 (Legambiente, 2020, Annual dossier series on air quality in Italy, referring the European Environmental Agency) relative to patients’ addresses over the last 5 years. Descriptive statistics and linear regression analyses were used to test the association between air pollutants levels and semen parameters.
Results: Overall, median (IQR) age and BMI were 37 (33-41) years and 24.3 (22.7-26.5) kg/m2, respectively. A CCI score = 1 was found in 98 (8.5%) men, and 318 (27.6%) participants were active smokers. Of 1152 men, 87 (7.6%) had normal sperm parameters. Of 1065 patients with abnormal semen analyses, 237 (22.3%), 324 (30.4%), and 287 (27.0%) patients presented 1, 2 or 3 abnormalities, respectively; 217 (20.38%) patients were azoospermic. At linear regression analysis, Pm10, Pm2.5, and NO2 were negatively associated with sperm morphology (Pm10: ß: -0.5288 µg/m3, p=0.001; Pm2.5: ß: -0.5240 µg/m3, p=0.019; NO2: ß: -0.4396 µg/m3, p<0.0001). Furthermore, the adjusted odds of sperm normal morphology <4% were 1.06 (95% CI 1.03-1.09; p=0.007) for Pm10, 1.07 (95% CI 1.03-1.11; p=0.007) for Pm 2.5, and 1.03 (95% CI 1.02-1.05; p=0.001) for NO2, respectively (Fig.1).
Conclusions: Findings of this cross-sectional study showed that Pm10, Pm 2.5, and NO2 levels were negatively associated with sperm morphology; conversely, they were not consistently associated with an increased risk of other abnormal sperm parameters in infertile men. Further studies are needed to better characterize air pollution effects on sperm parameters.
Source of Funding: None

.jpg)
.jpg)