Back
Poster, Podium & Video Sessions
Podium
PD20: Infertility: Epidemiology & Evaluation II
PD20-05: High prevalence of hormonal abnormalities in men without oligospermia
Saturday, May 14, 2022
7:40 AM – 7:50 AM
Location: Room 244
Matthew Hudnall*, Bailey Goyette, Minh Pham, Jeremy Lai, Justin Dubin, Chicago, IL, Richard Fantus, Evanston, IL, James Wren, Nelson Bennett, Robert Brannigan, Joshua Halpern, Chicago, IL
- MH
Podium Presenter(s)
Introduction: Newly updated male infertility guidelines from the American Urological Association recommend against universal hormone evaluation with measured levels of follicle stimulating hormone (FSH) and testosterone (T) in men with normal semen parameters due to prior limited data suggesting a low prevalence of abnormalities in this cohort. We sought to compare the prevalence of abnormal hormone parameters among men with and without sperm concentration abnormalities to determine the value of universal hormonal screening during fertility evaluation.
Methods: We retrospectively evaluated all men who underwent semen analysis (SA) and hormonal evaluation (morning serum T, FSH) at a large, integrated academic healthcare system between January 2002 and May 2021. Men were excluded if they had a prescription for T-modulating medications prior to index SA or if semen parameters were missing. Sperm concentration was dichotomized at 15 million/mL according to World Health Organization (WHO) criteria. Men with hormonal evaluation > 1 year following index SA were excluded. We compared median and interquartile range (IQR) T and FSH levels according to sperm concentration using Kruskal-Wallis test. Differences in prevalence of low testosterone ( <300 ng/dL) and abnormal FSH (>7.6 mIU/mL) were determined using Chi-square test.
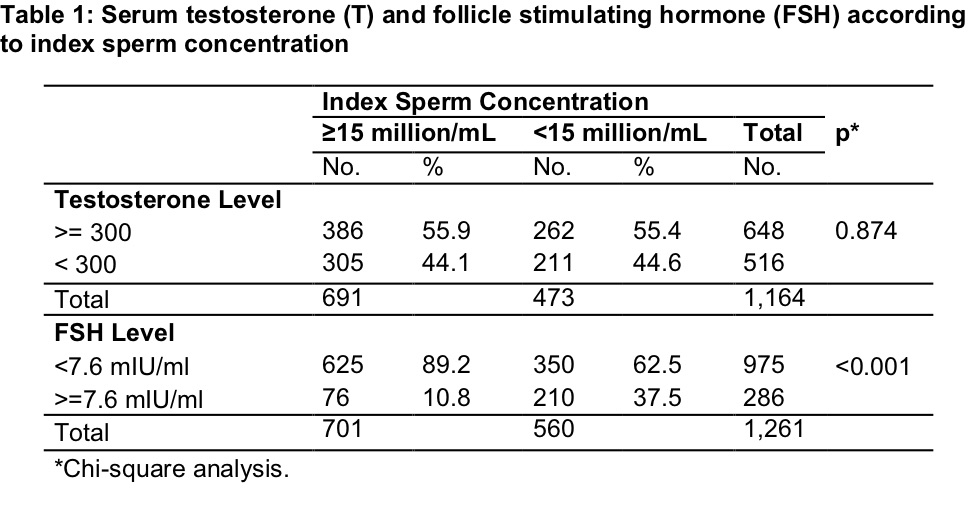
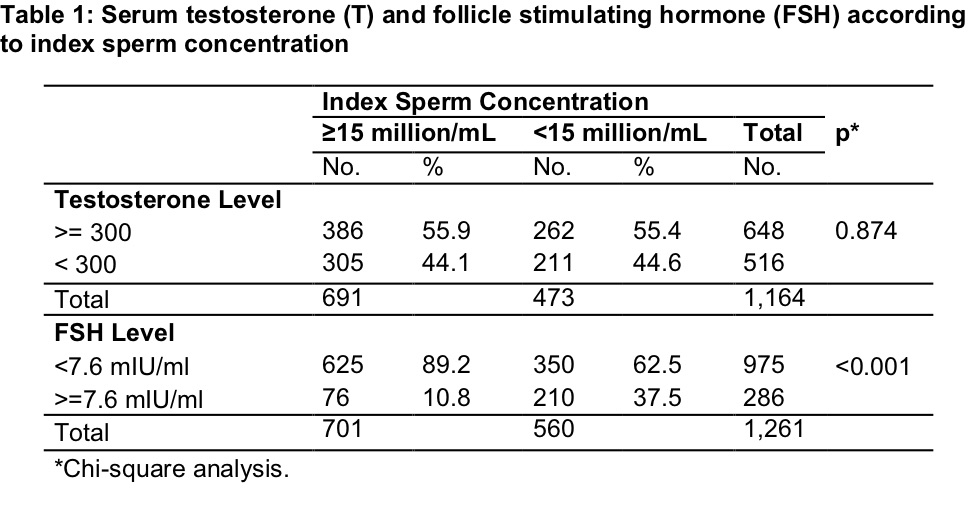
Results: A total of 1,164 men had a morning serum T. There was no difference in median T among men with normal vs abnormal sperm concentration (316 ng/dL, interquartile range [IQR] 250-399 vs 316 ng/dL, IQR [253-419]; p=0.515). FSH level was measured in 1,261 men. Median FSH was higher among men with sperm concentration <15 million/mL (6 IU/mL, IQR 3.85-10.7 vs 3.8 IU/mL, IQR 2.7-5.7; p<0.001). Among men with =15 million/mL concentration, 44.1% were found to have low T (p=0.874) and 10.8% had an FSH =7.6 mIU/mL (p < 0.001) (Table 1). Among men with =15 million/mL sperm concentration who underwent both T and FSH evaluation, 43.6% had at least 1 hormonal abnormality (Table 2).
Conclusions: A large percentage of men with normal semen analysis had low T, challenging prior literature. As low T may have long-term implications for both fertility and overall health, providers should consider universal T screening in men presenting for fertility evaluation.
Source of Funding: N/A
Methods: We retrospectively evaluated all men who underwent semen analysis (SA) and hormonal evaluation (morning serum T, FSH) at a large, integrated academic healthcare system between January 2002 and May 2021. Men were excluded if they had a prescription for T-modulating medications prior to index SA or if semen parameters were missing. Sperm concentration was dichotomized at 15 million/mL according to World Health Organization (WHO) criteria. Men with hormonal evaluation > 1 year following index SA were excluded. We compared median and interquartile range (IQR) T and FSH levels according to sperm concentration using Kruskal-Wallis test. Differences in prevalence of low testosterone ( <300 ng/dL) and abnormal FSH (>7.6 mIU/mL) were determined using Chi-square test.
Results: A total of 1,164 men had a morning serum T. There was no difference in median T among men with normal vs abnormal sperm concentration (316 ng/dL, interquartile range [IQR] 250-399 vs 316 ng/dL, IQR [253-419]; p=0.515). FSH level was measured in 1,261 men. Median FSH was higher among men with sperm concentration <15 million/mL (6 IU/mL, IQR 3.85-10.7 vs 3.8 IU/mL, IQR 2.7-5.7; p<0.001). Among men with =15 million/mL concentration, 44.1% were found to have low T (p=0.874) and 10.8% had an FSH =7.6 mIU/mL (p < 0.001) (Table 1). Among men with =15 million/mL sperm concentration who underwent both T and FSH evaluation, 43.6% had at least 1 hormonal abnormality (Table 2).
Conclusions: A large percentage of men with normal semen analysis had low T, challenging prior literature. As low T may have long-term implications for both fertility and overall health, providers should consider universal T screening in men presenting for fertility evaluation.
Source of Funding: N/A

.jpg)
.jpg)