Back
Poster, Podium & Video Sessions
Podium
PD20: Infertility: Epidemiology & Evaluation II
PD20-07: Elevated ROS levels and DNA fragmentation in sperm from convalescent men in SARS-CoV-2 infection.
Saturday, May 14, 2022
8:00 AM – 8:10 AM
Location: Room 244
Jorge Hallak*, Felipe Bernardes, Thiago Afonso Carvalho Celestino Teixeira, PAULO HILARIO NASCIMENTO SALDIVA, ESPER GEORGES KALLAS, ELIA TAMASO ESPIN GARCIA CALDINI, AMARO NUNES DUARTE NETO, HELOISA FAQUINETI, Vinicius Luiz Menezes Jesus, São Paulo, Brazil, RAUL SEGUNDO SANCHEZ GUTIERREZ, Temuco, Chile, Joel R Drevet, Clermont-Ferrand, France
- JH
Jorge Hallak, MD, PHD
Full Professor of Urology
Podium Presenter(s)
Introduction: Current evidence has proven the systemic nature of COVID19, including its involvement in the male reproductive tract. We aimed to investigate seminal parameters of moderate-to-severe COVID-19 men during the convalescence phase.
Methods: This cross-sectional study included 18 to 50-year-old men with confirmed moderate-to-severe COVID-19. Patients were enrolled 15 to 45 days after the diagnosis. After a urologist's initial clinical evaluation, semen samples were obtained by masturbation and processed within one hour. Semen analysis was performed using the World Health Organization (WHO) manual (6th edition). Sperm function tests were conducted in an andrology laboratory, including Reactive oxygen species (ROS), DNA fragmentation, lipid peroxidation, and Creatine Kinase (CK) analysis. An essential endocrine evaluation was performed. Patients with a history of disorders that could impair testicular function were excluded. A group of pre-vasectomy baseline samples was used as a control group. Statistical analysis was performed using R version 4.0.5. One-tailed and paired T-tests were used for comparisons between groups.
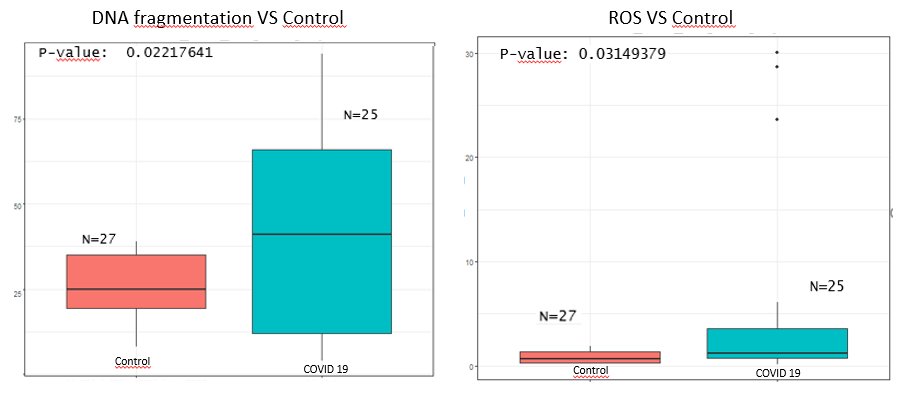
Results: The sample size was 26 men (mean 34.3 ± 6.5 years; range: 21–50 years). Sperm concentration (mean 38.74 ± 32, P<0.01) and total motile count (mean 55.3 ± 66.8, P<0.01) were significantly reduced in the COVID-19 group. The DNA fragmentation (mean 41.1 ± 29.2) and ROS (mean 4.84 ± 8.7) were significantly higher in post-infection patients. Other parameters such as WHO/Kruger morphology and progressive motility were also reduced in the disease group, albeit not statistically significant. Total testosterone (mean 409.2 ± 201.2) was lower in the convalescent men. All semen samples were negative for SARS-CoV-2 using the PCR analysis.
Conclusions: Our findings indicate that male reproductive injury can be a relevant component of SARS-CoV-2 systemic infection. High DNA fragmentation and ROS, hallmarks of tissue injury, might signal a direct testicular involvement. The morphological and functional damage could represent significant impairment of the male reproductive health if persistent after convalescence.
Source of Funding: None
Methods: This cross-sectional study included 18 to 50-year-old men with confirmed moderate-to-severe COVID-19. Patients were enrolled 15 to 45 days after the diagnosis. After a urologist's initial clinical evaluation, semen samples were obtained by masturbation and processed within one hour. Semen analysis was performed using the World Health Organization (WHO) manual (6th edition). Sperm function tests were conducted in an andrology laboratory, including Reactive oxygen species (ROS), DNA fragmentation, lipid peroxidation, and Creatine Kinase (CK) analysis. An essential endocrine evaluation was performed. Patients with a history of disorders that could impair testicular function were excluded. A group of pre-vasectomy baseline samples was used as a control group. Statistical analysis was performed using R version 4.0.5. One-tailed and paired T-tests were used for comparisons between groups.
Results: The sample size was 26 men (mean 34.3 ± 6.5 years; range: 21–50 years). Sperm concentration (mean 38.74 ± 32, P<0.01) and total motile count (mean 55.3 ± 66.8, P<0.01) were significantly reduced in the COVID-19 group. The DNA fragmentation (mean 41.1 ± 29.2) and ROS (mean 4.84 ± 8.7) were significantly higher in post-infection patients. Other parameters such as WHO/Kruger morphology and progressive motility were also reduced in the disease group, albeit not statistically significant. Total testosterone (mean 409.2 ± 201.2) was lower in the convalescent men. All semen samples were negative for SARS-CoV-2 using the PCR analysis.
Conclusions: Our findings indicate that male reproductive injury can be a relevant component of SARS-CoV-2 systemic infection. High DNA fragmentation and ROS, hallmarks of tissue injury, might signal a direct testicular involvement. The morphological and functional damage could represent significant impairment of the male reproductive health if persistent after convalescence.
Source of Funding: None

.jpg)
.jpg)