Back
Poster, Podium & Video Sessions
Podium
PD20: Infertility: Epidemiology & Evaluation II
PD20-10: Microsurgical Varicocelectomy is Associated with Improvement in Cap-ScoreTM and Probability of Generating a Pregnancy in Infertile Men
Saturday, May 14, 2022
8:30 AM – 8:40 AM
Location: Room 244
Jessica Marinaro*, Aaron Brant, Christopher Gaffney, Philip Xie, Nahid Punjani, Caroline Kang, Gianpiero Palermo, James Kashanian, NEW YORK, NY

Jessica A. Marinaro, MD
Fellow
MedStar Georgetown University Hospital
Podium Presenter(s)
Introduction: Poor sperm capacitation is a potential cause of male infertility. Sperm capacitation can be measured via an assay which evaluates monosialotetrahexosylganglioside (GM1) localization within the plasma membrane of human spermatozoa (Cap-Score™). We sought to determine if sperm capacitation would improve following varicocelectomy in infertile men.
Methods: We performed a prospective cohort study comparing pre- and post-operative semen analysis and Cap-Scores™ (Androvia LifeSciences) in men presenting to a single academic center with infertility from 1/2019 to 6/2021. We included men with unilateral or bilateral varicoceles determined by physical exam in the standing position who subsequently underwent microsurgical subinguinal varicocelectomy. Semen analyses were performed according to WHO (5th edition) criteria. We recorded semen volume, sperm concentration, motility, morphology, total motile sperm count (TMSC), Cap-ScoreTM and corresponding probability of generating a pregnancy (PGP) within 3 or fewer cycles of intrauterine insemination. We then compared pre- and post-operative values using Wilcoxon signed rank tests.
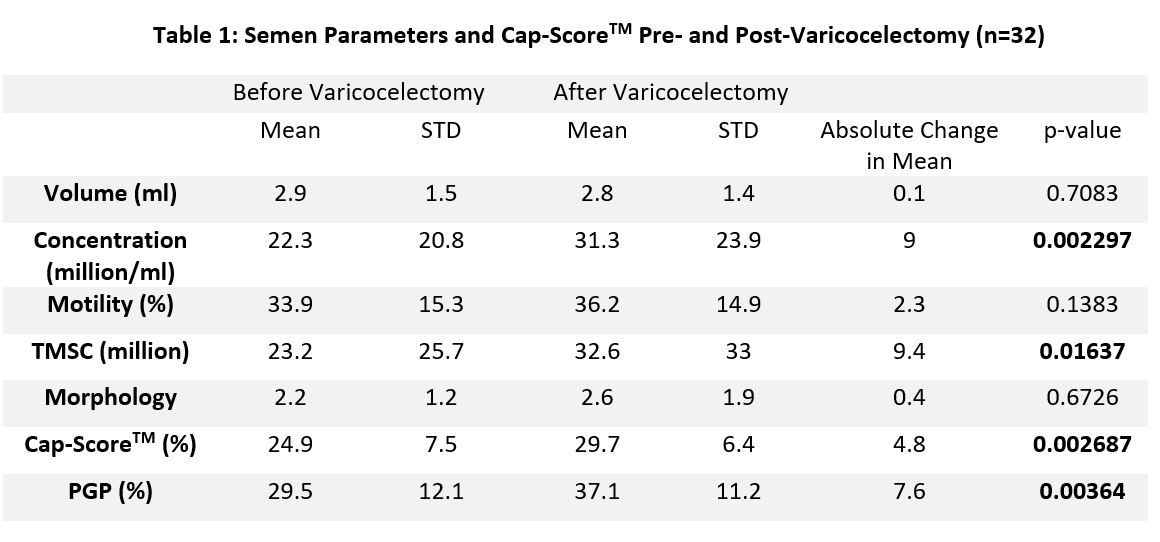
Results: Of the 126 men who underwent varicocelectomy from 1/2019 to 6/2021, we identified 32 (mean age 35.0 ± 5.3 years) who had a semen analysis and Cap-Score™ both before surgery and 3 months post-op (mean 111 ± 27 days) to allow a full cycle of spermatogenesis. Of these, 19/32 (59.4%) had bilateral varicoceles, 10/32 (31.3%) had a grade 2 varicocele and 16/32 (50%) had a grade 3 varicocele. There were no differences in semen volume, sperm motility, or sperm morphology after surgery; however, there was improvement in sperm concentration (p=0.002) and TMSC (p=0.02) (Table 1). Cap-ScoreTM and PGP improved in 25/32 men (78.1%). On average, Cap-ScoreTM increased 4.8% (p=0.003) and PGP increased 7.6% (p=0.004). On further analysis, the change in Cap-ScoreTM was not associated with a unilateral or bilateral repair, nor with varicocele grade (grade 1-2 vs grade 3).
Conclusions: Men treated with varicocelectomy have improvements in sperm concentration, TMSC, Cap-ScoreTM, and PGP as measured by Cap-ScoreTM. These results may have important implications for patient counseling and our understanding of how varicoceles alter sperm function.
Source of Funding: Authors JM and CK are supported in part by the Frederick J. and Theresa Dow Wallace Fund of the New York Community Trust
Methods: We performed a prospective cohort study comparing pre- and post-operative semen analysis and Cap-Scores™ (Androvia LifeSciences) in men presenting to a single academic center with infertility from 1/2019 to 6/2021. We included men with unilateral or bilateral varicoceles determined by physical exam in the standing position who subsequently underwent microsurgical subinguinal varicocelectomy. Semen analyses were performed according to WHO (5th edition) criteria. We recorded semen volume, sperm concentration, motility, morphology, total motile sperm count (TMSC), Cap-ScoreTM and corresponding probability of generating a pregnancy (PGP) within 3 or fewer cycles of intrauterine insemination. We then compared pre- and post-operative values using Wilcoxon signed rank tests.
Results: Of the 126 men who underwent varicocelectomy from 1/2019 to 6/2021, we identified 32 (mean age 35.0 ± 5.3 years) who had a semen analysis and Cap-Score™ both before surgery and 3 months post-op (mean 111 ± 27 days) to allow a full cycle of spermatogenesis. Of these, 19/32 (59.4%) had bilateral varicoceles, 10/32 (31.3%) had a grade 2 varicocele and 16/32 (50%) had a grade 3 varicocele. There were no differences in semen volume, sperm motility, or sperm morphology after surgery; however, there was improvement in sperm concentration (p=0.002) and TMSC (p=0.02) (Table 1). Cap-ScoreTM and PGP improved in 25/32 men (78.1%). On average, Cap-ScoreTM increased 4.8% (p=0.003) and PGP increased 7.6% (p=0.004). On further analysis, the change in Cap-ScoreTM was not associated with a unilateral or bilateral repair, nor with varicocele grade (grade 1-2 vs grade 3).
Conclusions: Men treated with varicocelectomy have improvements in sperm concentration, TMSC, Cap-ScoreTM, and PGP as measured by Cap-ScoreTM. These results may have important implications for patient counseling and our understanding of how varicoceles alter sperm function.
Source of Funding: Authors JM and CK are supported in part by the Frederick J. and Theresa Dow Wallace Fund of the New York Community Trust

.jpg)
.jpg)