Back
Poster, Podium & Video Sessions
Podium
PD21: Infections/Inflammation/Cystic Disease of the Genitourinary Tract: Kidney & Bladder II
PD21-10: Heterogeneity in the management of radiation-induced hemorrhagic cystitis
Saturday, May 14, 2022
8:30 AM – 8:40 AM
Location: Room 243
Brendan K. Wallace*, Anton M. Gillespie, George W. Moran, Michael B. Smigelski, Christopher B. Anderson, New York, NY
- BW
Podium Presenter(s)
Introduction: Radiation-induced hemorrhagic cystitis (HC) is a complication of pelvic radiotherapy, with an incidence of up to 5%. Though HC is often responsive to conservative measures, it can sometimes necessitate more complex therapies. There are no established guidelines for the pharmacological treatment of radiation-induced HC and there are few prospective studies examining the effectiveness of treatments. Our objective was to describe a cohort of refractory radiation cystitis patients and examine patterns of treatment and associated outcomes.
Methods: We conducted a retrospective cohort study to identify all patients from a single institution with radiation cystitis confirmed on cystoscopy who underwent pharmacological intervention for refractory hematuria from 2004 - 2019. Patient demographics, details of radiation therapy, and relevant admission data were collected. Initial conservative measures, such as continuous bladder irrigation (CBI), were noted, as well as the timing and sequence of subsequent pharmacological interventions. Descriptive statistics for continuous and categorical variables were summarized with median/interquartile range and numerical count/percentages, respectively.
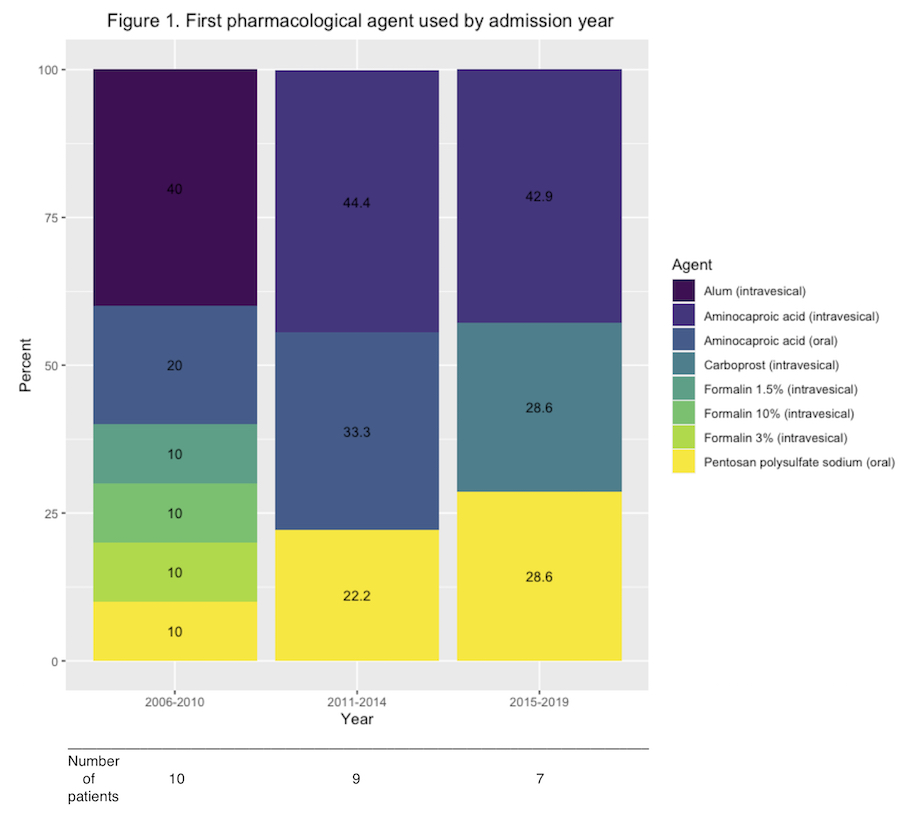
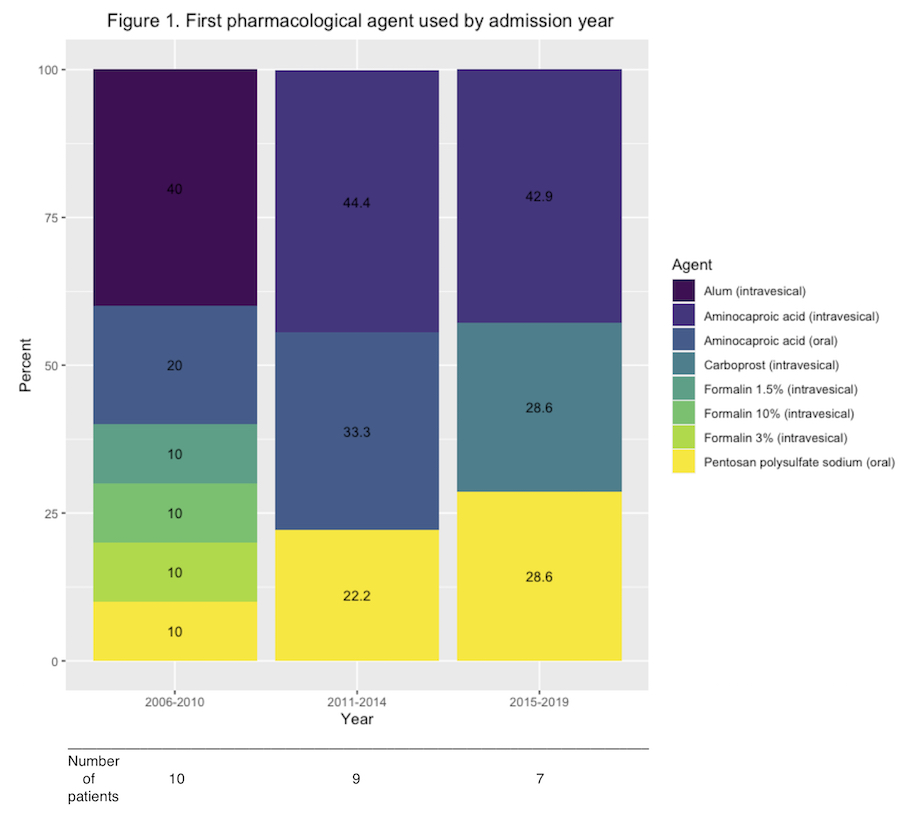
Results: We identified 23 patients with refractory hemorrhagic cystitis who were treated over 26 admissions. Most patients were male (91%), with a history of external beam radiation therapy (86%), primarily for prostate cancer (85%), and a median age of 73 (interquartile range [IQR]: 67 - 85). The majority of patients received a blood transfusion during their admission (88%) and 42% were initially in clot retention. Most patients received CBI before their first intervention (73%), for a median duration of 24 hours (IQR: 0 - 43). Eleven separate pharmacologic agents were used, with variations in the initial medication of choice over time (Figure 1). Most patients were treated with a combination of surgical and pharmacological interventions (85%), with 23% receiving a pharmacological agent before cystoscopy. The median length of stay was 9 days (IQR: 5 - 17), the 90-day readmission rate was 35%, and there was one in-hospital death (4%).
Conclusions: Pharmacologic treatment for refractory radiation-induced HC is inconsistent. Further work is needed to determine the optimal management strategy for this morbid complication.
Source of Funding: None
Methods: We conducted a retrospective cohort study to identify all patients from a single institution with radiation cystitis confirmed on cystoscopy who underwent pharmacological intervention for refractory hematuria from 2004 - 2019. Patient demographics, details of radiation therapy, and relevant admission data were collected. Initial conservative measures, such as continuous bladder irrigation (CBI), were noted, as well as the timing and sequence of subsequent pharmacological interventions. Descriptive statistics for continuous and categorical variables were summarized with median/interquartile range and numerical count/percentages, respectively.
Results: We identified 23 patients with refractory hemorrhagic cystitis who were treated over 26 admissions. Most patients were male (91%), with a history of external beam radiation therapy (86%), primarily for prostate cancer (85%), and a median age of 73 (interquartile range [IQR]: 67 - 85). The majority of patients received a blood transfusion during their admission (88%) and 42% were initially in clot retention. Most patients received CBI before their first intervention (73%), for a median duration of 24 hours (IQR: 0 - 43). Eleven separate pharmacologic agents were used, with variations in the initial medication of choice over time (Figure 1). Most patients were treated with a combination of surgical and pharmacological interventions (85%), with 23% receiving a pharmacological agent before cystoscopy. The median length of stay was 9 days (IQR: 5 - 17), the 90-day readmission rate was 35%, and there was one in-hospital death (4%).
Conclusions: Pharmacologic treatment for refractory radiation-induced HC is inconsistent. Further work is needed to determine the optimal management strategy for this morbid complication.
Source of Funding: None

.jpg)
.jpg)