Back
Poster, Podium & Video Sessions
Podium
PD22: Prostate Cancer: Localized: Radiation Therapy
PD22-01: Oncological Outcomes of Sentinel Lymph Node Procedure-Guided Radiotherapy versus Imaging-Guided Radiotherapy for Clinically Localized Prostate Cancer – a Multicenter, Retrospective, Propensity Score Weighted Comparison
Saturday, May 14, 2022
9:30 AM – 9:40 AM
Location: Room 252
Hilda de Barros*, Amsterdam, Netherlands, Nikolaos Grivas, Ioannina, Greece, Jan Duin, Daan Mulder, Vincent van der Noort, Amsterdam, Netherlands, Arjen Noordzij, Hoofddorp, Netherlands, Esther Wit, Eva Schaake, Pim van Leeuwen, Henk van der Poel, Amsterdam, Netherlands
- HD
Podium Presenter(s)
Introduction: Insufficient sensitivity of current imaging techniques for nodal staging has led to the exploration of the sentinel lymph node biopsy (SLNB) to select primary prostate cancer (PCa) patients that might benefit from whole-pelvic nodal radiotherapy (WPRT). In this study, we aimed to evaluate oncological outcomes of SLNB-based RT compared to imaging-based RT in cN0M0 PCa patients with an increased estimated risk of nodal metastases.
Methods: This multicenter, retrospective cohort study included 522 cN0 primary PCa patients with a Briganti nomogram-estimated nodal risk >5% treated with external beam RT (EBRT) between 2007-2018. Nodal staging was performed either by radiological staging (261 (50%) patients) or by radiological staging and an additional robot-assisted laparoscopic SLNB (261 (50%) patients). All patients received RT to the prostate and 6 months to 3 years of androgen deprivation therapy (ADT), whereas patients with a histologically positive sentinel node (pN1) also received RT to the pelvic LNs with 3 years of ADT. Endpoints included biochemical recurrence-free survival (BCR-FS) and radiological recurrence-free survival (RR-FS). Propensity score weighted (PSW) multivariable Cox regression analysis was performed to determine independent predictors of BCR and RR.
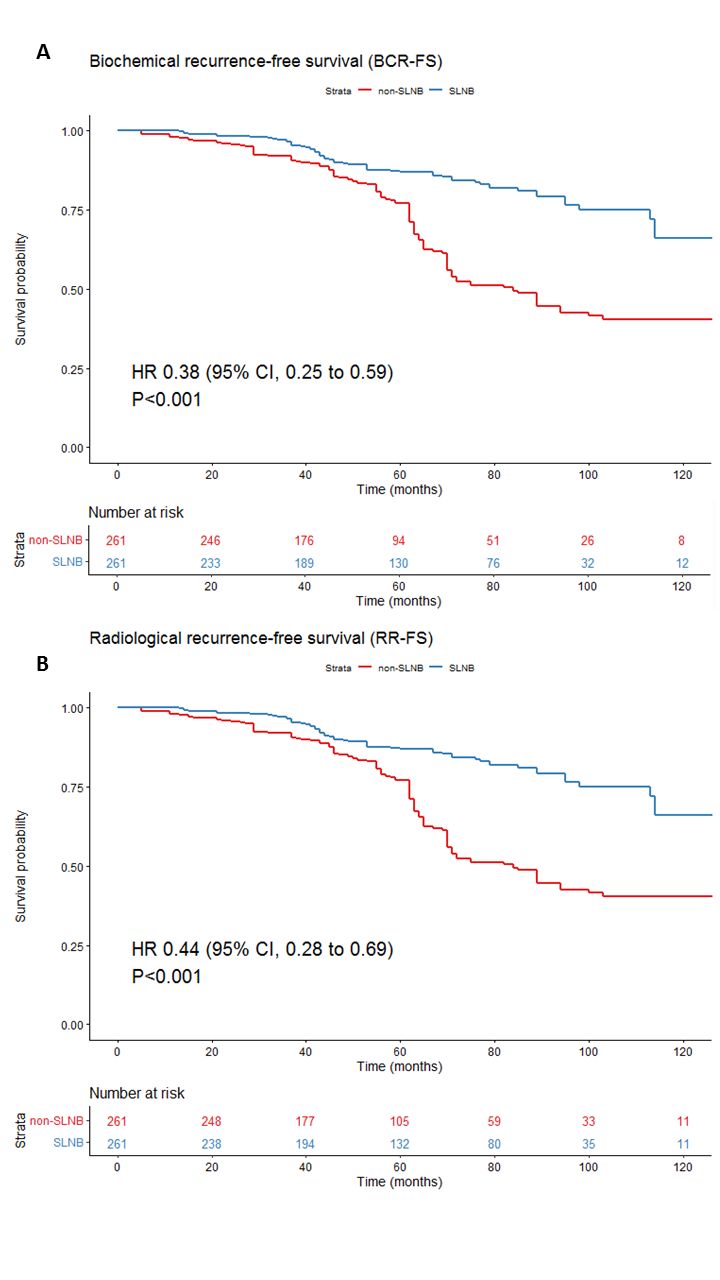
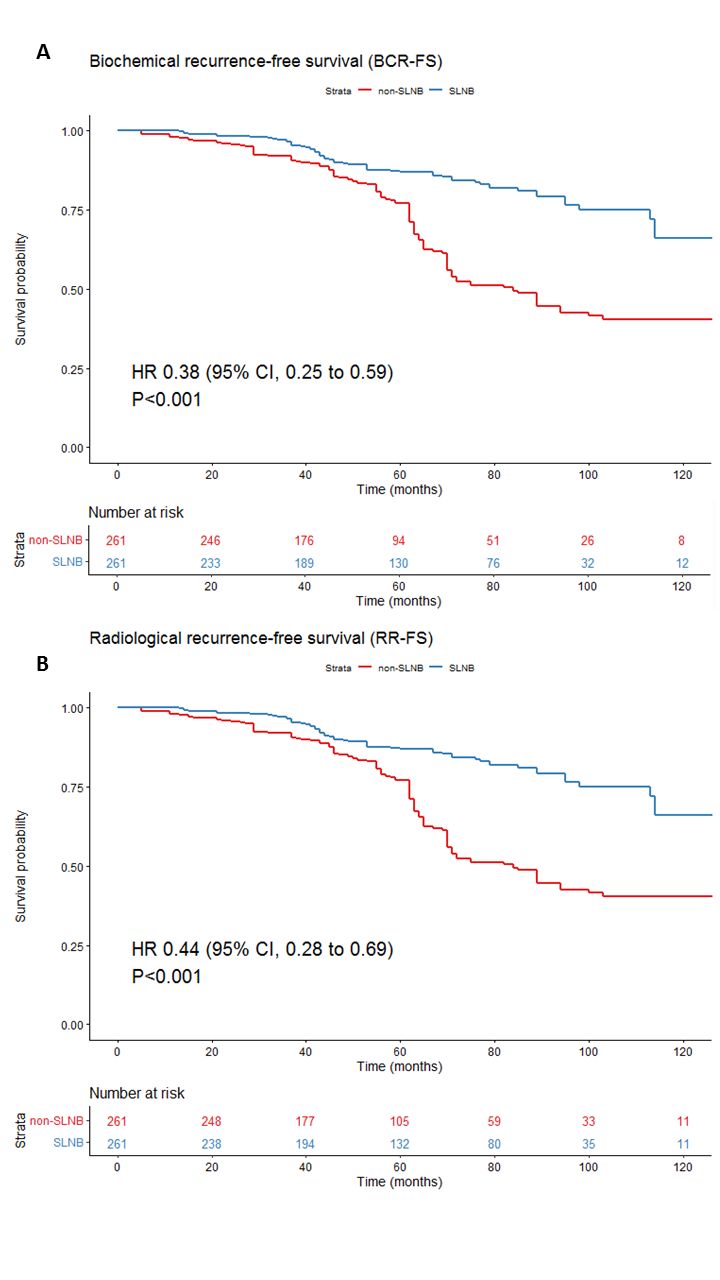
Results: Patients staged with SLNB had a higher rate of extracapsular extension (63% vs 35%, P <0.001) and were at higher risk of nodal metastases (43% vs 29%, P = 0.002) compared to imaging-only staged patients. Median follow-up after primary treatment was 64 months (IQR 41-95). In total, 111 patients developed a BCR (SLNB=51, non-SLNB=60) and 98 patients developed a radiological recurrence (SLNB=50, non-SLNB=48; Fig 1). In PSW multivariable Cox regression analyses, SLNB-based RT was an independent predictor of both BCR (HR 0.38, 95% CI 0.25-0.59, P <0.001) and RR (HR 0.44, 95% CI 0.28-0.69, P <0.001).
Conclusions: SLNB-guided RT is associated with a decreased risk of BCR and RR when compared to prostate-only RT in cN0 PCa patients. These results suggest an important role for SLNB in selecting cN0 PCa patients that might profit from WPRT and ADT intensification, and justify a prospective comparison.
Source of Funding: None
Methods: This multicenter, retrospective cohort study included 522 cN0 primary PCa patients with a Briganti nomogram-estimated nodal risk >5% treated with external beam RT (EBRT) between 2007-2018. Nodal staging was performed either by radiological staging (261 (50%) patients) or by radiological staging and an additional robot-assisted laparoscopic SLNB (261 (50%) patients). All patients received RT to the prostate and 6 months to 3 years of androgen deprivation therapy (ADT), whereas patients with a histologically positive sentinel node (pN1) also received RT to the pelvic LNs with 3 years of ADT. Endpoints included biochemical recurrence-free survival (BCR-FS) and radiological recurrence-free survival (RR-FS). Propensity score weighted (PSW) multivariable Cox regression analysis was performed to determine independent predictors of BCR and RR.
Results: Patients staged with SLNB had a higher rate of extracapsular extension (63% vs 35%, P <0.001) and were at higher risk of nodal metastases (43% vs 29%, P = 0.002) compared to imaging-only staged patients. Median follow-up after primary treatment was 64 months (IQR 41-95). In total, 111 patients developed a BCR (SLNB=51, non-SLNB=60) and 98 patients developed a radiological recurrence (SLNB=50, non-SLNB=48; Fig 1). In PSW multivariable Cox regression analyses, SLNB-based RT was an independent predictor of both BCR (HR 0.38, 95% CI 0.25-0.59, P <0.001) and RR (HR 0.44, 95% CI 0.28-0.69, P <0.001).
Conclusions: SLNB-guided RT is associated with a decreased risk of BCR and RR when compared to prostate-only RT in cN0 PCa patients. These results suggest an important role for SLNB in selecting cN0 PCa patients that might profit from WPRT and ADT intensification, and justify a prospective comparison.
Source of Funding: None

.jpg)
.jpg)