Back
Poster, Podium & Video Sessions
Podium
PD24: Urodynamics/Lower Urinary Tract Dysfunction/Female Pelvic Medicine: Neurogenic Voiding Dysfunction
PD24-07: Failure Rates of Bladder Outlet Surgeries for Stress Urinary Incontinence in Women with Neurogenic Lower Urinary Tract Dysfunction: A Multicenter Neurogenic Bladder Research Group Study dysfunction (NLUTD).
Saturday, May 14, 2022
10:30 AM – 10:40 AM
Location: Room 245
Javier Santiago*, Ann Arbor, MI, Min Soo Choo, Seoul, Korea, Republic of, Anne Cameron, Ann Arbor, MI, Richard Mora, Evgeniy Kreydin, David A Ginsberg, Los Angeles, CA, Natalia Hernandez, Paola Bustillos, Rose Khavari, Houston, TX, Stephanie Daignault-Newton, John Stoffel, Ann Arbor, MI
- JS
Javier E. Santiago, MD
Urology Resident
University of Michigan
Podium Presenter(s)
Introduction: We evaluated the outcomes of bladder outlet procedures for treating stress urinary incontinence (SUI) in female patients with neurogenic lower urinary tract dysfunction (NLUTD).
Methods: A retrospective multi-institutional study by the Neurogenic Bladder Research Group of female patients with NLUTD and SUI who underwent urethral bulking injection (UBI), pubovaginal sling (PVS), or artificial urinary sphincter (AUS) for (SUI) from 2012-2020 was performed via CPT and ICD-9 codes. Women undergoing concomitant bladder reconstruction or botulinum toxin (BTX) were included. The primary outcome was failure of bladder outlet procedure defined as return to pre-operative baseline SUI symptoms and/or needing additional surgical intervention for SUI. Time to failure were evaluated and multi-variable analysis for variables associated with failure were assessed.
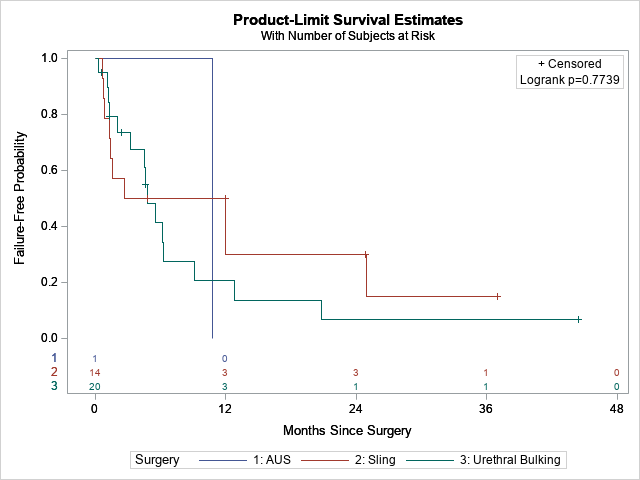
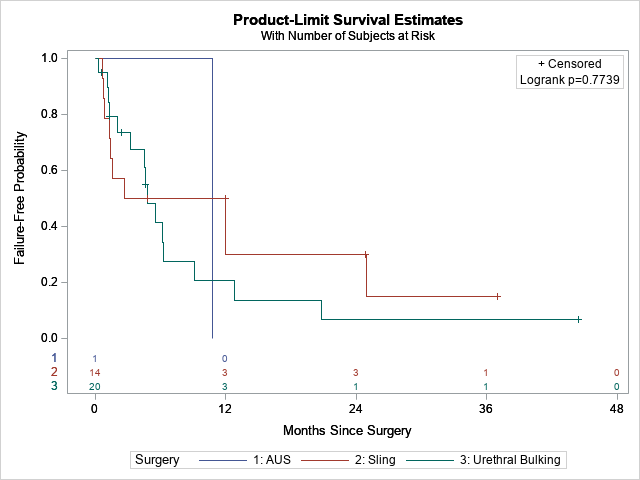
Results: Thirty-five female patients were included with diagnosis of spinal cord injury (35%), spina bifida (28%), and bladder exstrophy, multiple sclerosis or auto-immune neuropathy, pelvic surgery, or a supra-pontine disorder. There were 20, 14, and 1 cases of UBI, PVS, and AUS, respectively with a median follow up of 363 days. The median age was 46 years. BTX was performed exclusively with UBI (50%) and bladder reconstruction was performed more with sling vs UBI (29% vs 0%, p=0.02). Focusing on UBI and PVS, failure rates and time to failure between procedures were not significantly different on Kaplan Meier curves at median follow up of 5 and 14 months, respectively (75% failure at median 4.8 months for UBI vs 71% at 7.3 months for PVS, p=1). 6-month failure rates were 59% and 50% for UBI and PVS. Failure was only associated with increasing age on multivariable analysis. Additional surgeries for continence were performed in 60% and 57% patients after UBI and sling, respectively.
Conclusions: Urethral bulking agents and sling placement both demonstrated similarly low durability in managing SUI in NLUTD in this cohort, with the majority of patients requiring secondary surgeries for continence. This warrants further study to better understand factors impacting failure.
Source of Funding: None
Methods: A retrospective multi-institutional study by the Neurogenic Bladder Research Group of female patients with NLUTD and SUI who underwent urethral bulking injection (UBI), pubovaginal sling (PVS), or artificial urinary sphincter (AUS) for (SUI) from 2012-2020 was performed via CPT and ICD-9 codes. Women undergoing concomitant bladder reconstruction or botulinum toxin (BTX) were included. The primary outcome was failure of bladder outlet procedure defined as return to pre-operative baseline SUI symptoms and/or needing additional surgical intervention for SUI. Time to failure were evaluated and multi-variable analysis for variables associated with failure were assessed.
Results: Thirty-five female patients were included with diagnosis of spinal cord injury (35%), spina bifida (28%), and bladder exstrophy, multiple sclerosis or auto-immune neuropathy, pelvic surgery, or a supra-pontine disorder. There were 20, 14, and 1 cases of UBI, PVS, and AUS, respectively with a median follow up of 363 days. The median age was 46 years. BTX was performed exclusively with UBI (50%) and bladder reconstruction was performed more with sling vs UBI (29% vs 0%, p=0.02). Focusing on UBI and PVS, failure rates and time to failure between procedures were not significantly different on Kaplan Meier curves at median follow up of 5 and 14 months, respectively (75% failure at median 4.8 months for UBI vs 71% at 7.3 months for PVS, p=1). 6-month failure rates were 59% and 50% for UBI and PVS. Failure was only associated with increasing age on multivariable analysis. Additional surgeries for continence were performed in 60% and 57% patients after UBI and sling, respectively.
Conclusions: Urethral bulking agents and sling placement both demonstrated similarly low durability in managing SUI in NLUTD in this cohort, with the majority of patients requiring secondary surgeries for continence. This warrants further study to better understand factors impacting failure.
Source of Funding: None

.jpg)
.jpg)