Back
Poster, Podium & Video Sessions
Podium
PD25: Health Services Research: Practice Patterns, Quality of Life and Shared Decision Making II
PD25-03: Association Between Financial Burden and Treatment Regret in Men with Localized Prostate Cancer
Saturday, May 14, 2022
9:50 AM – 10:00 AM
Location: Room 244
Daniel D. Joyce*, Rochester, MN, Christopher J.D. Wallis, Toronto, Canada, Li-Ching Huang, Nashville, TN, Karen E. Hoffman, Houston, TX, Zhiguo Zhao, Tatsuki Koyama, Ralph Conwill, David F. Penson, Daniel A. Barocas, Nashville, TN

Daniel Joyce, MD
Mayo Clinic
Podium Presenter(s)
Introduction: We sought to understand the association between financial burden and treatment regret in men with localized prostate cancer to better understand the importance of inclusion of financial discussions in patient counseling.
Methods: Utilizing the multicenter, population-based Comparative Effectiveness Analysis of Surgery and Radiation (CEASAR) dataset, we identified all men accrued between 2011 and 2012 who underwent surgery, radiation, or active surveillance as primary management for localized prostate cancer. Patient-reported functional outcomes were assessed at baseline and longitudinally through 5 years using the 26-item Expanded Prostate Index Composite questionnaire. Treatment regret was assessed at 3- and 5-year follow-up using Clark’s validated scale. Financial burden was similarly evaluated at 3 and 5 years using a previously published 4-item questionnaire. The association between financial burden and treatment regret was assessed using multivariable logistic regression controlling for demographics, disease characteristics, treatment, functional outcomes, and patient expectations.
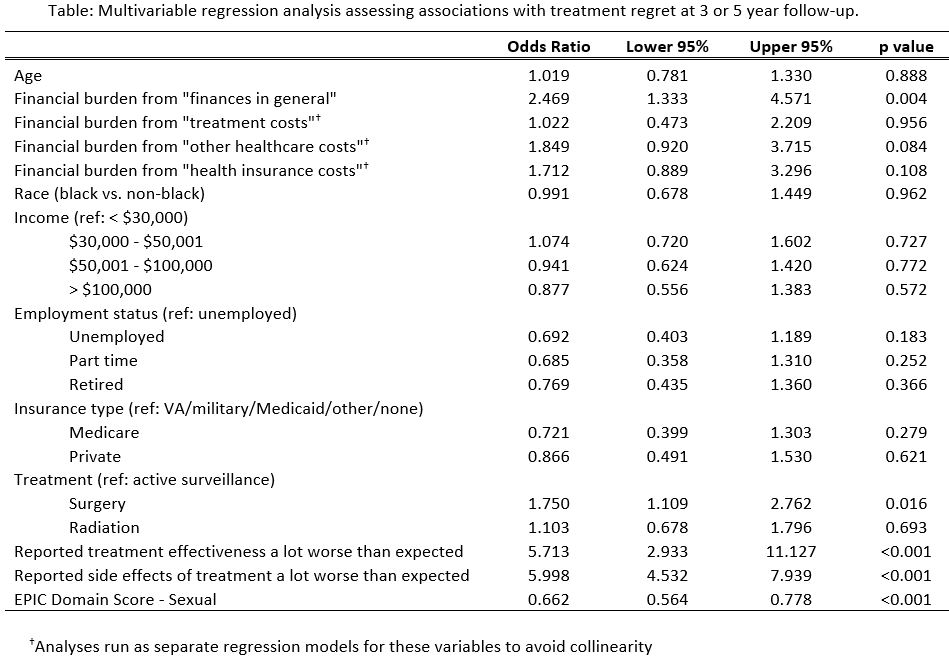
Results: Of the 2,924 men who met inclusion criteria, both regret and financial burden assessments were available for 80.6% (n=2,359). Prostate cancer management included surgery (n=1,256, 53.2%), radiation (n=787, 33.4%), and active surveillance (n=316, 13.4%). Financial burden from “finances in general” was associated with treatment regret at 3 and 5 years, after adjusting for potential confounders (OR 2.47, 95% CI 1.33, 4.57). Similar associations with financial burden from direct costs, such as treatment (OR 1.02, 95% CI 0.47, 2.21), clinic visit (OR 1.85, 95% CI 0.92, 3.71), and health insurance costs (OR 1.71, 95% CI 0.89, 3.30) were not observed (see table).
Conclusions: In this representative, population-based sample of men with localized prostate cancer, we observed associations between overall financial burden and treatment regret. The lack of association between treatment regret and measures of financial burden due to direct treatment costs may indicate a more profound impact on patients from indirect costs and should guide future efforts to address financial toxicity in prostate cancer management.
Source of Funding: This study was supported by the Agency for Healthcare Research and Quality (1R01HS019356, 1R01HS022640) and the Patient-Centered Outcomes Research Institute (CE-12-11-4667). Data management was facilitated by Vanderbilt University’s Research Electronic Data Capture (REDCap) system, which is supported by the Vanderbilt Institute for Clinical and Translational Research grant (UL1TR000011 from NCATS/NIH).
Methods: Utilizing the multicenter, population-based Comparative Effectiveness Analysis of Surgery and Radiation (CEASAR) dataset, we identified all men accrued between 2011 and 2012 who underwent surgery, radiation, or active surveillance as primary management for localized prostate cancer. Patient-reported functional outcomes were assessed at baseline and longitudinally through 5 years using the 26-item Expanded Prostate Index Composite questionnaire. Treatment regret was assessed at 3- and 5-year follow-up using Clark’s validated scale. Financial burden was similarly evaluated at 3 and 5 years using a previously published 4-item questionnaire. The association between financial burden and treatment regret was assessed using multivariable logistic regression controlling for demographics, disease characteristics, treatment, functional outcomes, and patient expectations.
Results: Of the 2,924 men who met inclusion criteria, both regret and financial burden assessments were available for 80.6% (n=2,359). Prostate cancer management included surgery (n=1,256, 53.2%), radiation (n=787, 33.4%), and active surveillance (n=316, 13.4%). Financial burden from “finances in general” was associated with treatment regret at 3 and 5 years, after adjusting for potential confounders (OR 2.47, 95% CI 1.33, 4.57). Similar associations with financial burden from direct costs, such as treatment (OR 1.02, 95% CI 0.47, 2.21), clinic visit (OR 1.85, 95% CI 0.92, 3.71), and health insurance costs (OR 1.71, 95% CI 0.89, 3.30) were not observed (see table).
Conclusions: In this representative, population-based sample of men with localized prostate cancer, we observed associations between overall financial burden and treatment regret. The lack of association between treatment regret and measures of financial burden due to direct treatment costs may indicate a more profound impact on patients from indirect costs and should guide future efforts to address financial toxicity in prostate cancer management.
Source of Funding: This study was supported by the Agency for Healthcare Research and Quality (1R01HS019356, 1R01HS022640) and the Patient-Centered Outcomes Research Institute (CE-12-11-4667). Data management was facilitated by Vanderbilt University’s Research Electronic Data Capture (REDCap) system, which is supported by the Vanderbilt Institute for Clinical and Translational Research grant (UL1TR000011 from NCATS/NIH).

.jpg)
.jpg)